Neurobiology of Sleep
7 min read Explore how the brain controls sleep, revealing the complex neurobiology behind restorative rest and its impact on health. (0 Reviews)
The Neurobiology of Sleep: Unlocking the Brain's Restorative Secrets
Sleep is one of the most mystifying and vital processes governing our daily lives. Despite spending roughly one-third of our lives asleep, the intricacies of how our brain orchestrates this state remain a remarkable field of scientific discovery. Understanding the neurobiology of sleep not only demystifies this complex phenomenon but also opens doors to improving health, cognition, and emotional well-being.
Introduction: Why Understanding Sleep Matters
Sleep has fascinated scientists for decades due to its critical role in memory consolidation, immune function, and mental health. In the words of renowned sleep researcher Dr. Matthew Walker, “The shorter your sleep, the shorter your lifespan.” This underscores why unraveling the brain’s control over sleep is essential in combating sleep disorders and their associated health risks such as obesity, depression, and neurodegenerative diseases.
Brain Structures: The Sleep Command Centers
The control of sleep arises from a carefully balanced interplay between various brain regions. Among these, the hypothalamus stands out as a pivotal regulator. Within it lies the suprachiasmatic nucleus (SCN), often called the brain's 'master clock.' The SCN synchronizes sleep patterns with the external light-dark cycle by regulating circadian rhythms.
Another key player is the brainstem, especially the pontine and medullary regions, which control transitions between the distinct phases of sleep—Rapid Eye Movement (REM) and Non-Rapid Eye Movement (NREM) sleep. For example, neurons in the pontine tegmentum have been shown to generate REM sleep by activating mechanisms responsible for vivid dreaming and muscle atonia.
The thalamus acts as a relay hub modulating sensory input to the cortex during sleep, essentially filtering out external stimuli. This enables the brain to enter a peaceful state despite environmental interruptions.
Neurotransmitters and Chemicals: The Molecular Regulators
Neurotransmitters orchestrate the delicate dance between wakefulness and sleep. Gamma-aminobutyric acid (GABA), the principal inhibitory neurotransmitter, plays a critical role in initiating and maintaining sleep by dampening neuronal excitability.
Conversely, wakefulness-promoting neurotransmitters like orexin (also known as hypocretin) are crucial for keeping us alert. Malfunction or deficiency in orexin production is the biological basis for narcolepsy, a disorder characterized by sudden sleep attacks.
Histamine and acetylcholine are also important; histaminergic neurons in the hypothalamus maintain cortical arousal, while acetylcholine has a complex role, enhancing REM sleep and promoting cortical activation.
Neural Circuits: Transitioning Between Sleep Stages
Sleep is not a homogeneous state but cycles through distinct stages: NREM stages 1-3 and REM sleep. Each stage involves unique neural circuit activities and functional roles.
In deep NREM sleep (slow-wave sleep), synchronized neuronal oscillations occur across cortex and thalamus, thought to underlie memory consolidation and synaptic homeostasis. For instance, studies have shown that the hippocampus replays neuronal patterns during slow-wave sleep to consolidate recent experiences into long-term memory.
Transitioning to REM sleep, brain circuits involving the pons activate cholinergic neurons triggering rapid eye movements, vivid dreaming, and heightened brain activity resembling wakefulness. However, the spinal cord is inhibited, preventing muscle movement and ensuring the body remains immobile.
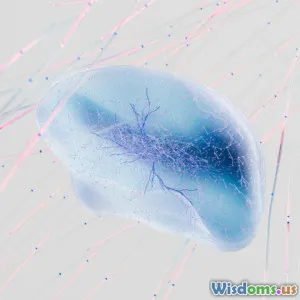
The Glymphatic System: The Brain’s Nighttime Cleaner
A groundbreaking discovery in recent years is the glymphatic system, which becomes highly active during sleep. Acting as a waste clearance pathway, it flushes out metabolic toxins such as beta-amyloid—a protein linked to Alzheimer’s disease.
This function is predominantly active during slow-wave sleep, emphasizing the importance of deep sleep for long-term brain health and preventing neurodegenerative disorders.
Real-World Implications and Applications
Understanding neurobiology has transformed clinical approaches to sleep disorders. For example, the discovery of orexin's role led to the development of orexin receptor antagonists as novel sleep medications. Drugs like suvorexant target orexin receptors to promote sleep by inhibiting wakefulness pathways.
Furthermore, knowledge about circadian rhythms has led to strategies like timed light exposure to treat conditions like delayed sleep phase disorder and jet lag.
Research also informs cognitive-behavioral therapy for insomnia (CBT-I), which addresses dysfunctional behaviors and reinforces natural sleep processes rather than relying solely on pharmacological means.
Conclusion: Sleeping Smarter Through Science
The neurobiology of sleep reveals a complex yet elegant system of brain networks, chemical messengers, and physiological processes harmonizing to sustain both rest and awakening. Modern science not only unravels these mechanisms but empowers us to leverage this understanding for better health, enhanced learning, and disease prevention.
As emerging research continues to decode how sleep influences every facet of brain function and body health, prioritizing quality sleep is increasingly recognized not as a luxury but a neurological necessity. Through informed practices, medical advances, and public awareness, we can harness the power of sleep to unlock improved well-being and cognitive vitality.
“Sleep is the single most effective thing we can do to reset our brain and body health each day.” — Matthew Walker, Why We Sleep
References:
- Walker, M. P. (2017). Why We Sleep: Unlocking the Power of Sleep and Dreams. Scribner.
- Saper, C. B., Scammell, T. E., & Lu, J. (2005). Hypothalamic regulation of sleep and circadian rhythms. Nature.
- Xie, L. et al. (2013). Sleep drives metabolite clearance from the adult brain. Science.
- Taheri, S. et al. (2002). Hypocretins/Orexins and sleep. Nature Reviews Neuroscience.
Rate the Post
User Reviews
Popular Posts