Ten Surprising Ethical Dilemmas Faced by Doctors Worldwide
15 min read Explore ten lesser-known ethical dilemmas that challenge doctors in diverse medical environments around the globe. (0 Reviews)
Ten Surprising Ethical Dilemmas Faced by Doctors Worldwide
The world places doctors on a high pedestal, picturing them as impartial healers devoted solely to saving lives. Yet, behind a stethoscope often lies a world filled with ambiguity and challenging choices. Ethical dilemmas stretch far beyond dramatic tales sometimes depicted in fiction; they're interwoven into the day-to-day reality of practicing physicians, regardless of country or specialty. Here are ten nuanced, thought-provoking ethical predicaments that influence the journey of doctors across the globe.
Navigating Patient Confidentiality in the Digital Age

The principle of patient confidentiality has underpinned medical ethics for centuries. However, the mass adoption of electronic health records and cloud-based hospital systems adds complexity. Doctors today frequently wrestle with questions like: Who precisely should have access to patient files? Is it justifiable to override privacy in the interest of family safety or public health?
Consider the dilemma faced when a patient admits to having a contagious disease like tuberculosis, but refuses to allow notification of her household or employer. In some regions, laws require reporting to health authorities, but disclosure might affect her employment and relationships. Similarly, hospitals increasingly share data across networks, sometimes with less-than-perfect cybersecurity. In 2023, a major data breach in Australia exposed information from over 1 million patients, triggering debates about how much responsibility providers should take for these breaches.
Doctors constantly juggle between following the letter of the law, respecting patient autonomy, and contributing to public welfare—all while navigating imperfect digital infrastructures.
Resource Allocation in Low-Income Settings

Imagine running an ER in a disaster zone, or a rural hospital with only two ventilators and five critical patients. How does one prioritize care ethically when resources don't match needs? While triage protocols exist, they can become murky in gray-area cases.
Doctors in Sub-Saharan Africa, during the 2014 Ebola outbreak, had to choose which patients received limited anti-viral medication—decisions that meant, inevitably, some would be denied care. During the COVID-19 pandemic, similar ethical triage played out globally, with Italian ICUs openly discussing criteria such as age and comorbidity. The emotional toll on providers in these gut-wrenching circumstances can linger for years.
Moreover, such resource allocation dilemmas thrust doctors into the uncomfortable role of gatekeepers, often forced to factor in age, disability, or likelihood of recovery—areas fraught with significant bias risk and ethical discomfort.
Dealing with Demands for Non-Evidence-Based Treatments
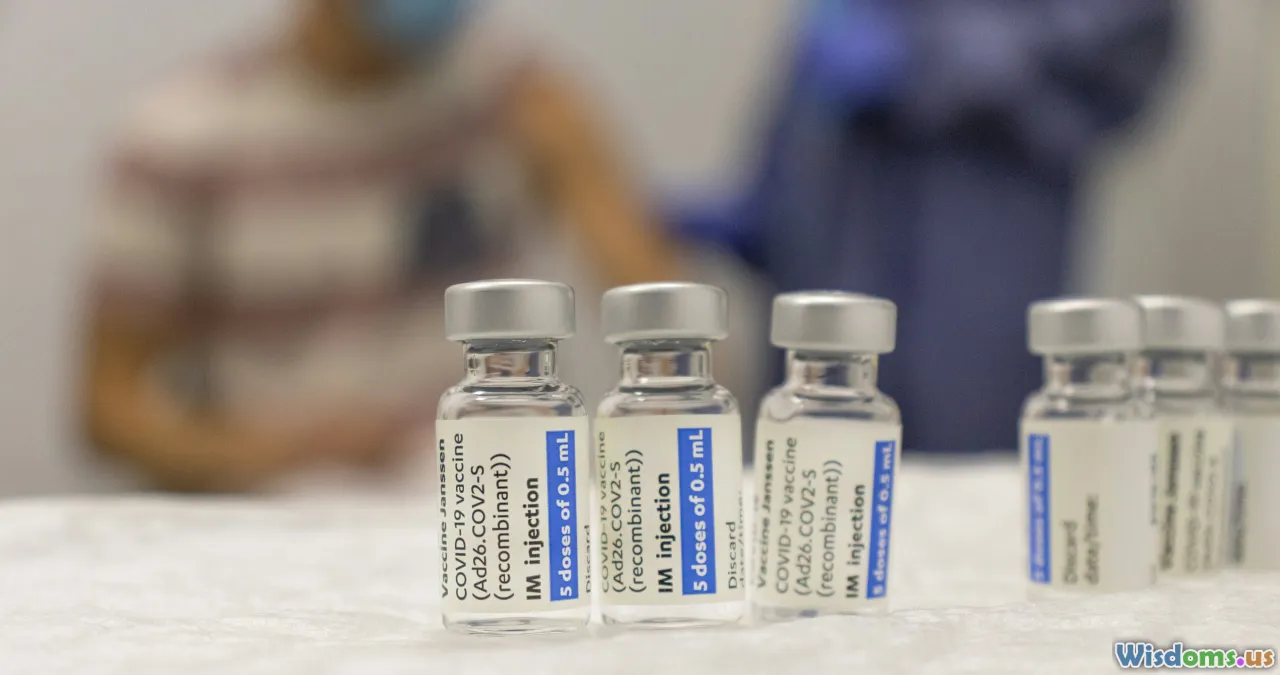
The rise of social media and online health communities has emboldened patients to demand specific treatments—sometimes ones not backed by robust evidence. Doctors face a dilemma between respecting patient autonomy and advocating for evidence-based practice.
A notable example arose with the anti-vaccine movement and, more acutely, during the COVID-19 crisis. Physicians encountered countless requests for hydroxychloroquine or ivermectin despite insufficient scientific endorsement. Even outside pandemics, oncologists may battle pressure to recommend unproven alternative cancer remedies because of online testimonials.
Should doctors comply to keep their patients' trust, or refuse and risk fracturing the therapeutic alliance? Medical councils advise transparency and education, but the right course is not always clear—especially in communities where refusing non-evidence care might damage a clinician's reputation and income.
Treating Family Members or Close Friends

Every doctor receives requests to "just write a prescription" for a spouse or sibling. While providing care might appear compassionate or convenient, it risks impairing objectivity and professional boundaries.
Ethical guidelines, such as those set by the American Medical Association and General Medical Council, generally discourage treating those with whom one has a close personal relationship, except in emergencies. For example, in 2021, a UK GP was reprimanded for orchestrating her partner's medication refill—an act that sidestepped critical monitoring steps. The emotional stakes are high when a loved one's health hangs in the balance: doctors may struggle to say no, risking both regulatory penalty and personal fallout.
Involvement in End-of-Life Decisions and Physician-Assisted Dying

End-of-life decisions are among the most searing dilemmas doctors encounter. Some countries have legalized physician-assisted dying under strict protocols (Netherlands, Canada, several US states), leading to complex clinical, legal, and moral issues.
What if a terminally ill patient, in unbearable pain, demands assistance in ending their life? Should a doctor follow law or personal conscience, particularly in nations where such practices are still illegal or culturally taboo?
In Belgium, at least 2,400 euthanasia cases were recorded in 2022, with some physicians choosing to conscientiously object, transferring the patient’s care. Meanwhile, in places lacking legal guidance, such as Nigeria or the Middle East, covert decisions are made to withhold or withdraw aggressive treatment—sometimes without a formal ethical framework, raising concerns about transparency and patient autonomy.
Doctors must reconcile personal beliefs, regulatory duties, and compassion for patients and families—a balancing act prone to deep introspection and, sometimes, public controversy.
Addressing Cultural and Religious Conflicts

Cultural and religious values heavily influence perceptions of health and treatment. Doctors often face the challenge of respecting diverse traditions while advocating for effective care.
For example, some Jehovah’s Witnesses decline blood transfusions, even if life-saving, based on religious doctrine. In India, women from some conservative backgrounds may refuse examinations by male doctors unless a female is present, which can slow emergency care.
Medical pluralism (using both traditional and modern medicine) further complicates matters. Doctors must tread delicately—educating without alienating, offering options that align as closely as possible with patient values, and, ultimately, supporting informed refusal when appropriate. These scenarios underscore the need for cultural competence and humility in contemporary practice.
Facing the Reality of Medical Corruption and Bribery

Corruption in healthcare manifests in many guises, from under-the-table payments for expedited services to influence in procurement of drugs. In parts of Eastern Europe and South Asia, small "gifts" to a doctor aren't just common—they're expected.
Doctors who refuse such practices may face resentment or even professional isolation. A 2018 study revealed that in Lithuania, nearly 20% of hospital patients reported giving bribes for preferential treatment. Conversely, taking bribes can result in disciplinary action or loss of license, as happened in China in a well-publicized 2019 case involving senior oncologists.
Courage is required to defy ingrained systems of gift-giving, yet the dilemma rarely has a neat solution, especially for junior staff reliant on established structures for career advancement.
Treating Unrepresented or Vulnerable Patients

Doctors are frequently called to care for patients who cannot make decisions for themselves—those incapacitated by dementia, substance use, or mental illness. But who consents when there are no family or legal proxies? This challenge, known as the "unrepresented patient" dilemma, is growing in developed and developing worlds alike.
In the United States, hospitals sometimes convene ethics panels to advise treatment for such patients. Yet, these bodies may lack clear legal authority or the nuanced understanding requisite for each case. In countries without such structures, doctors may have no choice but to proceed based on clinical judgment, risking legal repercussions if their actions are later disputed.
One telling example arose during Hurricane Katrina, when overwhelmed doctors made difficult triage calls for sedated, unresponsive patients left behind in floodwaters—decisions later scrutinized both legally and ethically.
Struggles with Medical Futility and Family Wishes

Sometimes, life-prolonging interventions offer negligible chances of recovery but are still fiercely desired by patients' families, often for spiritual or emotional reasons. The question of "medical futility" arises most often in ICUs, where ventilators and medications keep organs functioning long after chances of meaningful survival have waned.
A well-publicized 2018 case in London involved a toddler, Alfie Evans, whose parents contested the hospital’s plan to withdraw life support, resulting in a high-profile legal battle. Doctors must negotiate between evidence, empathy, and legal constraints, facing unjust accusations of heartlessness if they recommend withdrawing care.
In Japan, surveys suggest over 50% of ICU physicians have continued invasive care against their best judgment because of family insistence. These situations are deeply distressing for all involved, underscoring the limits of even the most advanced medicine in bringing clarity to emotionally complex decisions.
Managing Conflict of Interest in Clinical Trials and Research
Progress in medicine relies on robust clinical trials. Yet doctors worldwide sometimes struggle to avoid conflicts of interest, especially when funded by pharmaceutical companies.
Physicians participating in trials must always prioritize patient welfare over potential personal or institutional gain. This became clear in the infamous Vioxx case, when suppressed negative data on cardiovascular risk led to widespread harm before the drug was pulled from the market.
Policy dictates doctors disclose relationships with sponsors, but enforcement can be inconsistent. In 2022, an Indian investigation revealed physicians receiving significant payments for enrolling patients in device studies of questionable benefit, despite nominal institutional oversight. Managing transparency with patients—and resisting the lure of industry-sponsored incentives—remains an ongoing challenge.
Every ethical dilemma faced by physicians is unique but shares a familiar core: the constant negotiation between personal conscience, professional ethics, legal boundaries, and patient need. As global healthcare further entangles with technology, commerce, and cultural shifts, the importance of wisdom, humility, and self-reflection in medical decision-making has never been greater. Recognizing, discussing, and addressing these dilemmas openly is a crucial step toward a more equitable and compassionate health system for all.
Rate the Post
User Reviews
Popular Posts