What Happens If the Thalamus Shuts Down
15 min read Explore the vital role of the thalamus and the consequences if it shuts down. (0 Reviews)
The Silent Gatekeeper: What Happens If the Thalamus Shuts Down
Imagine a complex city at the heart of your brain, bustling with information and activity, juggling massive amounts of sensory signals every moment. This city is the thalamus—a small, paired structure crucial to how we experience and respond to the world. But what would happen if, suddenly, the thalamus went dark? Understanding this scenario is more than a theoretical exercise; it exposes just how pivotal the thalamus is to our consciousness, movement, emotion, and very sense of being. Let's explore what unfolds if the thalamus, the brain’s silent gatekeeper, ceases to function.
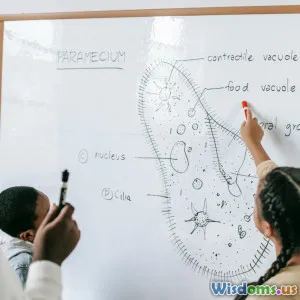
Anatomy & Role of the Thalamus
The thalamus sits deep within the center of the brain, shaped much like two small eggs perched atop the brainstem. It acts as a hub, relaying information between various regions of the brain and the spinal cord. All sensory signals, except for smell, first pass through this structure before reaching the cerebral cortex—the brain's outer layer that deciphers and weighs responses.
Clinical studies underscore that the thalamus isn't just a messenger; it sorts, processes, and emphasizes what matters. For example, when you touch a hot stove, pain signals flash to the thalamus, which then prioritizes them, sending a "pay attention!" alert to your cortex. Conversely, if you're lost in thought, the thalamus can downplay background noise, helping you focus on a good book. This filtering process is essential; without it, the brain would be eternally overwhelmed by raw sensory chaos, unable to respond meaningfully.
Thalamic Shutdown: Medical Perspectives

A complete shutdown of the thalamus, thankfully, is a rare medical event. However, cases of stroke, traumatic injury, and certain viral infections offer a glimpse into its effects. For instance, bilateral thalamic infarction—an event where both thalamic bodies are damaged due to interrupted blood flow—often results in coma or persistent vegetative states. These outcomes arise because the thalamus is critical for maintaining consciousness and arousal.
In severe thalamic injury, patients often exhibit loss of all sensory inputs except olfaction (the sense of smell)—the only system bypassing the thalamus entirely. Neurologists report that these patients do not respond to touch, pain, or even see and hear, as these signals can't reach the conscious mind. Notably, in clinical tests such as the Glasgow Coma Scale, patients with nonfunctional thalami typically score extremely low, reflecting the loss of arousal and awareness.
Consciousness and The Thalamus
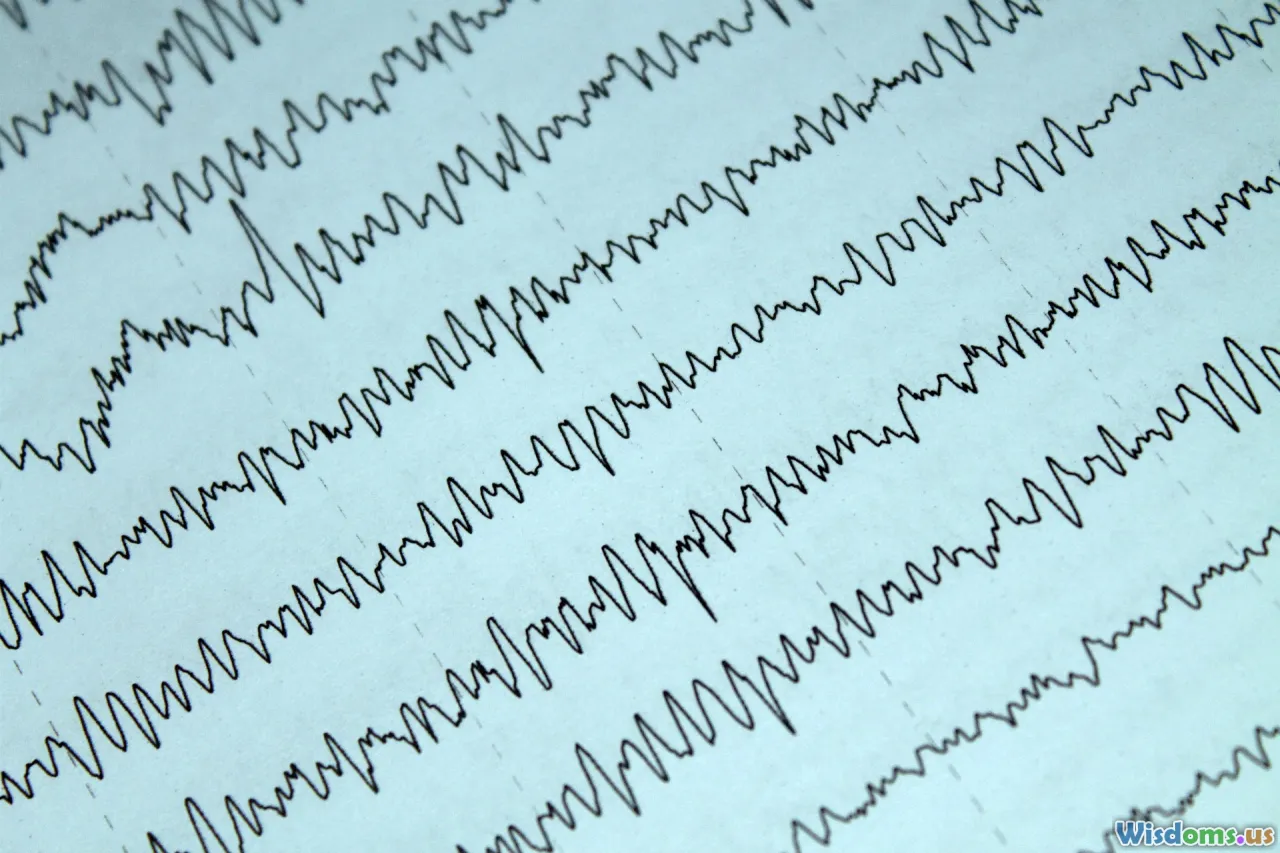
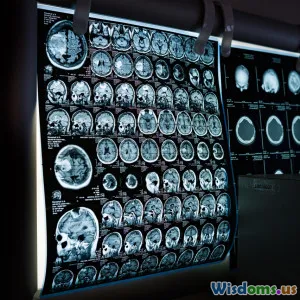
The thalamus is perhaps most famous for its role in consciousness. This isn’t just speculation—animal studies and brain imaging in humans show thalamic activity surging during waking states and plummeting during sleep or anesthesia. Scientists determined that the thalamus and its extensive network with the cortex form what’s known as the "thalamocortical loop." Without this feedback circuit, coherent consciousness collapses.
Consider the experience of anesthesia. Dr. Emery Brown, an anesthesiologist and neuroscientist, notes that drugs used during surgery often target the thalamus to induce unconsciousness. MRI scans reveal that as patients fall asleep or are anesthetized, thalamic activity decreases correspondingly. When the thalamus is reactivated, consciousness returns.
This insight underpins the tragic mechanics of a vegetative state, where thalamic function may be selectively destroyed. In one pivotal study (Laureys et al., Science, 2000), patients in persistent vegetative states were found to have massive thalamic damage, with the remaining cortex largely intact—a sobering reminder of how this small region anchors our sense of self.
Sensory Overload and Gatekeeping

Life without the thalamic filter would mean relentless, unfiltered sensory input—a scenario captured hauntingly in some severe neurological conditions. With a failing thalamus, the brain loses its ability to prioritize sensory information. The result? Overwhelming, chaotic perception, if consciousness is even retained.
Music therapist Dr. Oliver Sacks documented patients suffering from thalamic lesions who described vivid, intrusive hallucinations. These experiences arose because sensory gating—filtering irrelevant stimuli—had failed, so the brain compensated by concocting its own reality out of the confusion. While such cases are rare, they underscore just how the thalamus orchestrates the symphony of the senses, preventing cognitive "noise" from disrupting focus and awareness.
Motor Control and Coordination

It’s not just perception and consciousness—move your hand or walk across the room, and the thalamus is hard at work. This nucleus relays information between the motor cortex and the body, crucial for fine-tuning movement and balance.
In diseases like Parkinson’s, parts of the thalamus malfunction. Patients experience tremors, rigidity, and bradykinesia (slowness of movement). Targeted deep-brain stimulation of thalamic nuclei can sometimes alleviate these motor symptoms, demonstrating the thalamus's essential calibration role. If the thalamus were to shut down completely, voluntary movement would cease—the brain could no longer coordinate signals to or from the muscles. This total body paralysis, combined with unconsciousness, resembles the locked-in syndrome, though with an even deeper lack of responsiveness.
Emotional and Cognitive Fallout
The thalamus connects not only to sensory and motor areas but also to regions governing emotion, learning, and memory. Functional MRI studies show that when we experience joy, fear, or sadness, the thalamus integrates these emotional cues and ties them to memories. For example, seeing a childhood playground might spark nostalgia—this link is impossible without the thalamic relay.
A disrupted thalamus has been implicated in psychiatric illnesses. Schizophrenia offers a telling case: postmortem and imaging studies find thalamic anomalies in many patients, correlated with disordered thinking and hallucinations. It remains unclear if thalamic dysfunction is the root cause or an effect, but the relationship is strong enough that psychiatrists now look for subtle thalamic changes when diagnosing complex mood and cognitive disorders.
Sensory Exceptions: Why Smell Survives

Perhaps the most fascinating quirk of thalamic function is its exclusion from the sense of smell. All other senses travel through the thalamus, but olfactory nerves lead directly from the nasal passages to the cortex. Evolutionary biologists speculate this is due to smell being one of the earliest-developed senses, predating the thalamus's role as a central relay.
This means, in rare circumstances of thalamic shutdown, a patient might still respond (at least at a neural, if not conscious, level) to powerful odors. Unique case studies highlight individuals with severe thalamic strokes recognizing the smell of burnt toast or flowers, but unable to process sights, sounds, or touch. It’s a faint echo of their former multisensory existence.
Real-Life Case Studies

Medical history documents astonishing cases illustrating the thalamus's importance. In 1941, Baron Constantin von Economo described a mysterious epidemic, encephalitis lethargica, where patients suffered drowsiness drifting into coma. Autopsies later revealed widespread thalamic damage.
Another contemporary example involves Wendy, a patient whose bilateral thalamic stroke left her in a minimally conscious state. Upon targeted neuro-rehabilitation that stimulated adjacent regions and engaged her sense of smell (her only preserved sense), she regained slivers of awareness. While full recovery was elusive, her case illuminated efforts to bypass or supplement thalamic circuits—a focus for research into recovery after brain injury.
Thalamic Stimulation: A Ray of Hope

Thanks to advances in neuroscience, some promising therapies may partially rescue lost thalamic function. Deep brain stimulation (DBS) involves implanting electrodes into the brain, including the thalamus. Originally used in movement disorders like Parkinson's, DBS has been tested in restoring consciousness in minimally responsive patients. In a 2007 study published in Nature, rigorous stimulation of thalamic areas led to noticeable improvements in awareness and functional abilities, though much work remains to fine-tune these interventions.
Cutting-edge research also explores noninvasive stimulation, such as applying magnetic fields to thalamic regions through the scalp, seeking to "jump-start" dormant circuits. Early results suggest that these techniques, while not a panacea, could offer rays of hope for patients languishing between coma and wakefulness.
Lessons from the Thalamus: Actionable Takeaways

The scenario of thalamic shutdown is a haunting, poignant window into how collective brain functions underpin who we are. While catastrophic shutdown is rare, it’s a clarion call for protecting brain health. Here are actionable tips inspired by the thalamus’s vital role:
- Prioritize Sleep: Research shows chronic sleep deprivation reduces thalamic activity and compromises attention, mood, and memory. Aim for 7–9 hours to fuel optimal brain relay.
- Safeguard Against Stroke: Hypertension and diabetes commonly cause thalamic strokes. Regular checkups, diet adjustments, and exercise are simple but effective protective measures.
- Practice Mindfulness: Focusing your attention through meditation has been shown to alter thalamic pathways, improving sensory filtering and enhancing emotional regulation.
- Learn Continuously: Engaging in cognitive challenges and social activities maintains thalamic-cortical agility, helping prevent age-related decline.
Recognizing warning signs like sudden changes in sensation, movement, or consciousness is vital. Swift medical intervention can sometimes prevent irreversible thalamic damage.
The Thalamus: A Critical Crossroads

The thalamus may be a small structure amidst the grand architecture of the brain, but its influence is both overarching and intimate. Without its harmonious relay, our sensory experience fragments, motor functions crumble, emotions disconnect—all leading to the collapse of consciousness itself.
By appreciating the thalamus’s sweeping duties, we glimpse the wonders of healthy brain function, and the fragility imposed by its sudden loss. As research advances, new therapies may one day harness or circumvent these networks, bringing renewed hope to those affected. Until then, nurturing brain health and understanding warning signs are the best safeguards for the gatekeeper within.
Rate the Post
User Reviews
Popular Posts