The Future of Healthcare Automation
9 min read Explore how healthcare automation is transforming patient care, improving efficiency, and shaping the future of medicine. (0 Reviews)
The Future of Healthcare Automation
Healthcare is on the cusp of a revolutionary transformation, fueled by rapid advancements in automation technologies. From robotic-assisted surgeries to AI-driven diagnostics and patient monitoring systems, automation promises to bring unprecedented improvements in quality, efficiency, and accessibility. But what does the future hold for healthcare automation? This in-depth exploration unpacks the emerging trends, real-world applications, challenges, and potential paradigms reshaping medicine in the 21st century.
Introduction: Automation at the Crossroads of Medicine and Technology
Imagine a hospital where repetitive administrative tasks are effortlessly handled by AI, diagnostics are made with unparalleled accuracy, and treatments are tailored through machine intelligence. This isn’t science fiction—these developments are rapidly approaching. The global healthcare automation market, valued at approximately $14 billion in 2020, is projected to expand at a CAGR of over 8% through 2030 (Grand View Research). This growth reflects technology's growing imprint on medicine, promising to reduce human error, cut costs, and enhance patient outcomes.
However, alongside these opportunities lie critical ethical, practical, and technical challenges that healthcare stakeholders must navigate carefully.
Automation in Diagnosis: AI and Machine Learning at Work
One of the most impactful aspects of healthcare automation lies in diagnostic technologies powered by artificial intelligence (AI) and machine learning algorithms. Automated diagnostic tools can analyze vast medical datasets—imaging, pathology slides, genetic profiles—with speed and precision beyond human capabilities.
Real-World Example: AI in Radiology
Deep learning models can identify anomalies in radiologic scans. For instance, Google Health’s AI demonstrated radiology-level accuracy in detecting breast cancer from mammograms, reducing false positives and negatives substantially (Nature, 2020). Similarly, automated interpretation of CT scans during the COVID-19 pandemic helped triage patients and detect complications quickly.
By automating initial analysis, radiologists can focus on complex cases, enhancing throughput and accuracy.
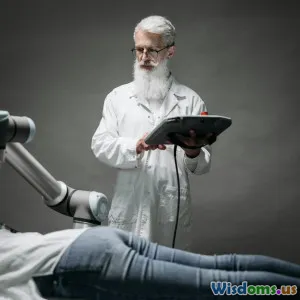
Robotics in Surgery: Precision Meets Automation
Robotic surgery systems, like the da Vinci Surgical System, exemplify automation’s potential to augment surgical precision and reduce invasiveness.
Benefits and Innovations
Robotic-assisted procedures enable finer motor control and tremor filtration, allowing minimally invasive operations, fewer complications, and faster recovery. Advances such as autonomous robot suturing and AI-powered intraoperative decision support are emerging frontiers.
Moreover, telesurgery—remote robotic surgeries—can expand expert care access to underserved regions. For example, surgical robots are being tested in remote areas, potentially overcoming geographical disparities.
Automation in Administrative Tasks: Streamlining Healthcare Operations
Beyond clinical care, automation is revolutionizing healthcare administration—one of the most time- and resource-heavy areas.
Electronic Health Records (EHR) Automation
Natural language processing (NLP) automates documentation by transcribing and interpreting physician-patient interactions in real time. It reduces physician burnout from paperwork and ensures consistent record accuracy.
Billing and Scheduling Automation
Automated billing systems enhance accuracy, reduce fraud, and accelerate claims processing. AI-driven patient scheduling ensures optimal resource allocation, balancing patient load and minimizing wait times.
A report by the American Medical Association highlights that physicians spend up to two hours on administrative tasks for every hour of patient care—automation can greatly rebalance this ratio.
Remote Monitoring and Wearables: Continuity of Care Beyond the Clinic
Automation in healthcare extends outside hospitals through wearable devices that continuously monitor vital parameters like heart rate, glucose levels, and oxygen saturation.
Example: Continuous Glucose Monitoring
For diabetes management, devices like Dexcom G6 automate real-time glucose tracking and alert patients and clinicians about dangerous fluctuations, reducing hospitalizations.
AI-Enabled Remote Patient Monitoring
Platforms using AI analyze trends in monitored data, predict health deteriorations, and prompt early interventions. This proactive approach exemplifies a shift toward value-based care replacing episodic, reactive models.
This technology particularly benefits chronic disease management, post-operative care, and elderly patients aiming to age in place safely.
Data Integration and Interoperability: The Backbone of Healthcare Automation
The full potential of automation relies on seamless data integration. Healthcare data often exist in silos—laboratory, imaging, pharmacy records—posing barriers to effective automation.
The Role of Interoperability Standards
HL7 FHIR (Fast Healthcare Interoperability Resources) standards are crucial in enabling different systems to communicate effectively, allowing AI algorithms and automation tools to process holistic patient information, not just isolated data points.
This interoperability fosters comprehensive decision-making, better population health insights, and scalable automation solutions.
Challenges and Ethical Considerations
The promise of automation is tempered by concerns:
- Data Privacy and Security: Protecting sensitive health information amid increased digital automation is paramount.
- Job Displacement: Automation may disrupt healthcare jobs, requiring workforce retraining.
- Algorithmic Bias: AI systems may perpetuate biases if trained on unrepresentative datasets, negatively impacting marginalized populations.
- Regulatory and Liability Issues: Determining responsibility when automated systems make errors remains complex.
Addressing these challenges requires multi-stakeholder collaboration involving policymakers, technologists, clinicians, and patients.
Looking Ahead: A Vision for the Next Decade
As automation technologies mature, integrating human expertise with machine efficiency will create hybrid care models excelling in empathy, precision, and accessibility. Emerging trends include:
- Personalized Medicine: AI-driven genomics will customize therapies at the individual level.
- Autonomous Diagnostics: Fully automated diagnostic centers capable of providing rapid, accurate results without human intervention.
- Virtual Health Assistants: AI companions supporting patient adherence and wellness, improving chronic disease management.
The COVID-19 pandemic accelerated digital transformation, highlighting automation’s critical role in scalable healthcare delivery.
Quote to Ponder
"Healthcare is entering an era where automation will not replace the human touch; instead, it will amplify clinicians' ability to provide personalized, efficient, and accessible care."—Dr. Alicia Chen, HealthTech Innovator
Conclusion
Healthcare automation stands at the nexus of technology and humanity, driving a future where patient care is enhanced through smart machines and AI-driven processes. While challenges exist, thoughtful implementation grounded in ethics and human-centric design can make healthcare more efficient, accurate, and inclusive.
By embracing this technological evolution, we can create systems that do not just manage disease but holistically support health and well-being globally.
The future of healthcare is automated, intelligent, and compassionate—and it begins today.
References
- Grand View Research, "Healthcare Automation Market Size, Share & Trends Analysis Report, 2021-2030."
- McKinney SM et al., "International evaluation of an AI system for breast cancer screening." Nature (2020).
- The American Medical Association, "Physician Burnout and Administrative Burden.", 2021.
- HL7 International, "FHIR Overview."
- Dexcom, "Continuous Glucose Monitoring Systems."
Rate the Post
User Reviews
Popular Posts



















