The Science Behind Flare Ups and How to Prevent Them
14 min read Explore the science behind flare ups and discover evidence-based strategies to prevent them in chronic conditions. (0 Reviews)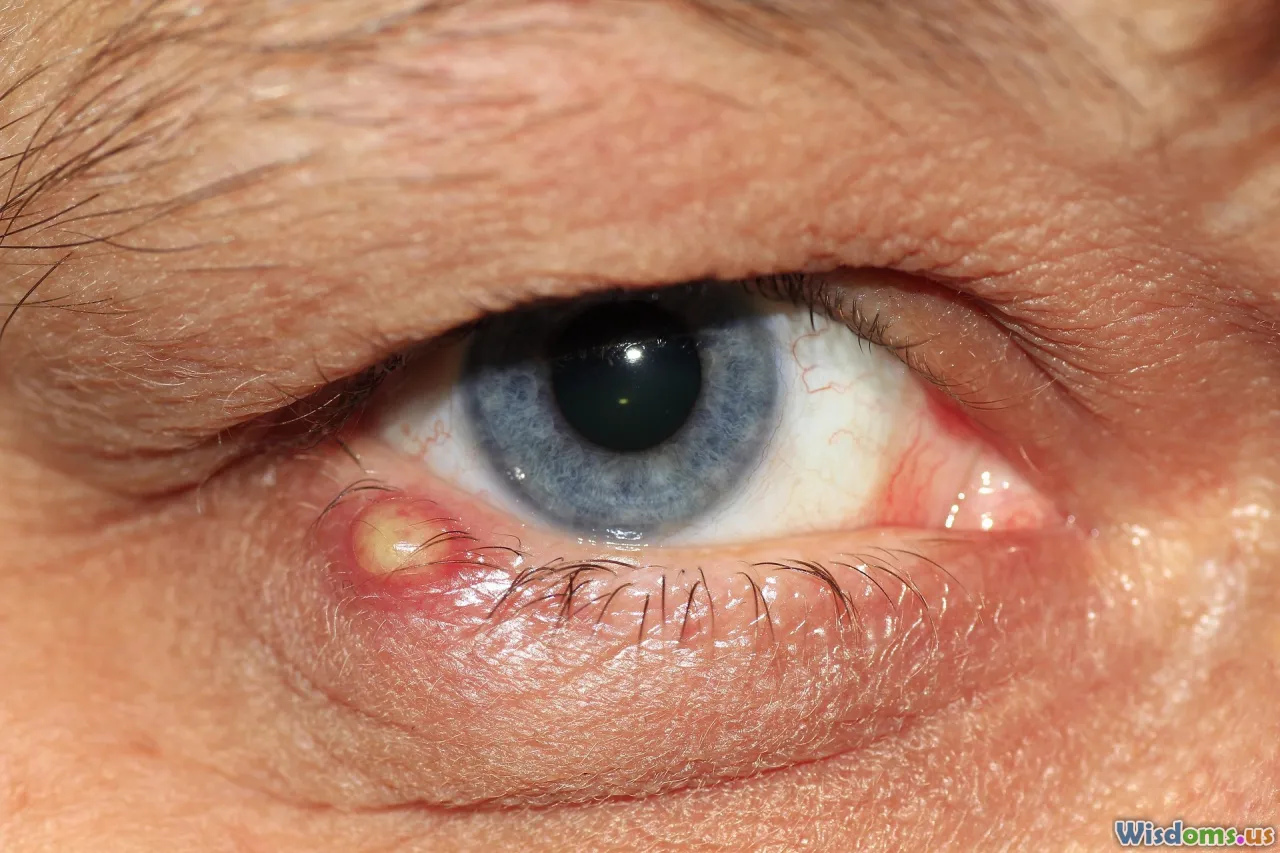
The Science Behind Flare Ups and How to Prevent Them
Flare ups can be a source of frustration and concern, whether you 2re dealing with a chronic illness, allergies, or common skin conditions. These sudden exacerbations aren 2t just inconvenient 7they can hinder daily life and signal underlying health issues. But what causes flare ups, and is it possible to prevent them? Let 2s delve into the science behind these episodes, providing an actionable guide for keeping symptoms at bay.
Understanding Flare Ups: What Happens in Your Body

At the heart of every flare up is a complex interplay between environmental factors, bodily processes, and sometimes, genetic predispositions. Fundamentally, a flare up refers to a sudden and significant worsening of symptoms in chronic conditions such as eczema, asthma, rheumatoid arthritis, or irritable bowel syndrome.
The Immune System's Role
Most flare ups are rooted in the immune system. In autoimmune diseases like lupus or rheumatoid arthritis, the body mistakenly attacks itself, triggering inflammation. For instance:
- In eczema (atopic dermatitis), skin barriers weaken, inviting irritants or allergens to provoke immune responses. This initiates an itch-scratch cycle, fueling more inflammation and skin damage.
- In asthma, airborne triggers cause airways to constrict and inflame, making breathing difficult.
Chemical Messengers and Inflammation
Cytokines are tiny proteins released during an immune response. When the body detects danger 7rue or false 7it releases cytokines that summon more immune cells, creating redness, heat, swelling, or pain. Chronic elevations of these molecules can lead to frequent or severe flare ups.
Real-World Example: The Eczema Itch Cycle
A 2021 study in the Journal of Allergy and Clinical Immunology revealed that scratching due to even mild eczema rapidly releases histamine and interleukins, worsening symptoms. Breaking this cycle is key to preventing flare ups in atopic dermatitis.
Common Triggers that Cause Flare Ups
Identifying your personal flare up triggers can feel like detective work 7rials, tracking, and sometimes frustrating mistakes. However, certain triggers commonly cause exacerbations in chronic illnesses.
Environmental Factors
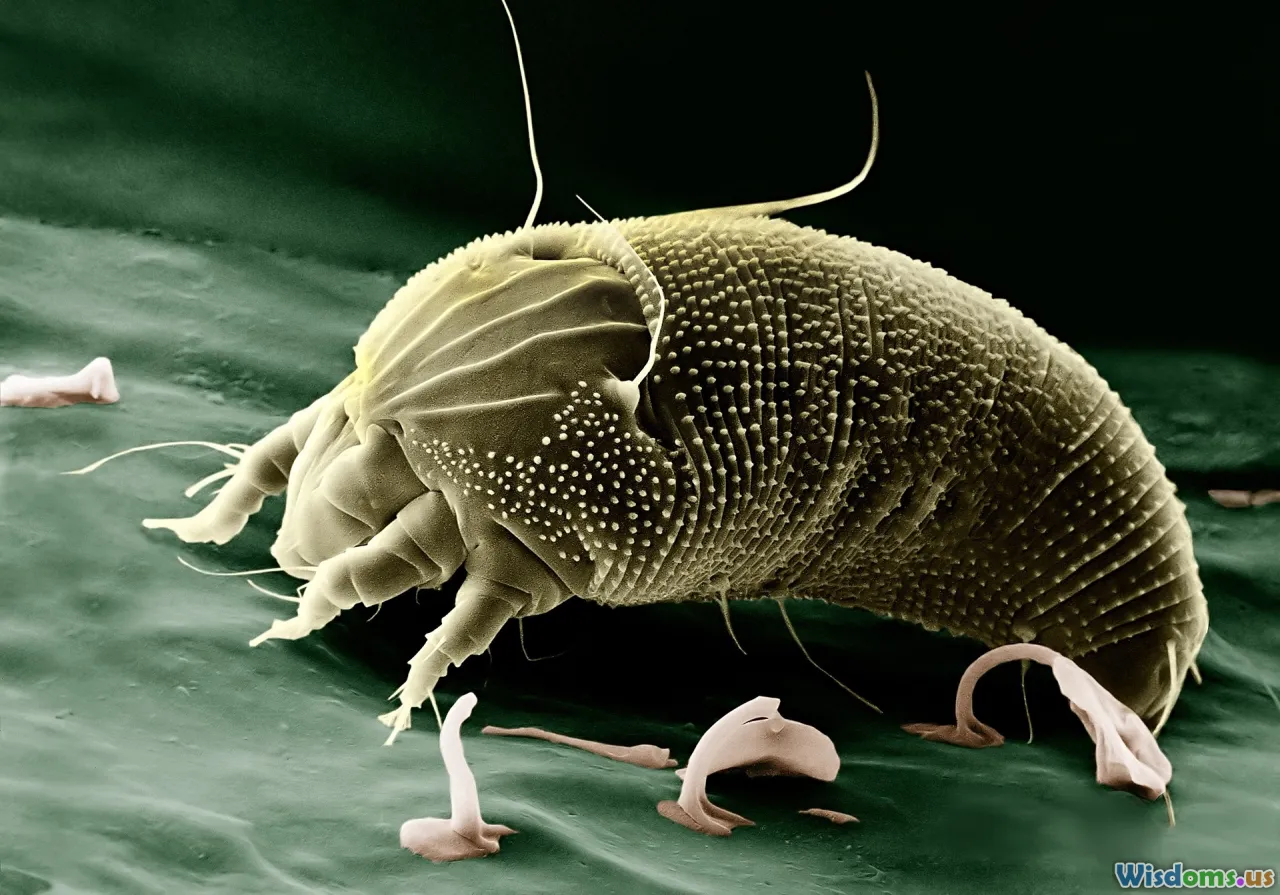
- Allergens: Dust mites, pet dander, mold, and pollen are notorious for igniting flare ups in asthma and allergies. Geographic location and weather conditions can further amplify these effects.
- Temperature Changes: Sudden shifts from hot to cold 7or vice versa 7can provoke skin and respiratory flare ups due to vascular or bronchial sensitivity.
Lifestyle Triggers
- Diet: Flare ups of gout, eczema, or irritable bowel syndrome are often connected to specific foods (e.g., shellfish, high-sugar foods, dairy, or gluten).
- Stress: Psychological stress has been well-documented to trigger immune responses, precipitating everything from migraines to inflammatory bowel disease (IBD) attacks.
Medication and Hormones
Even seemingly unrelated medications (like non-steroidal anti-inflammatory drugs for heart disease) may induce asthma flare ups. Hormonal shifts, such as those during menstruation or pregnancy, frequently affect autoimmune and skin disorders.
Case Example: A study in the UK among asthmatics discovered that over 70% experienced flare ups during high pollen seasons, but those monitoring indoor humidity and using air filters had significantly fewer attacks.
Diagnosing a Flare Up: When and How to Seek Help
It can sometimes be difficult to distinguish a flare up from normal fluctuations in symptoms. Recognizing warning signs early can prevent minor annoyances from becoming major health crises.
Key Signs of a Flare Up
- Sudden swelling, pain, or redness in affected joints or skin areas
- Increased severity/frequency of baseline symptoms: e.g., needing reliever inhalers more often
- Unusual fatigue, fever, or weight changes
When to Call a Doctor
- If symptoms progress rapidly or are unresponsive to usual treatments
- Development of new symptoms (e.g., fever with redness in autoimmune diseases)
- Difficulty breathing, chest pain, or high fevers 7hese are urgent symptoms
Quick Tip: Starting a daily symptom and trigger journal (using apps like Symple or mySymptoms) helps patients and clinicians identify patterns, facilitating better treatment choices.
The Science of Prevention: How to Minimize Your Flare Up Risk

Preventing flare ups is not just about avoiding triggers 7it's about strengthening your body's resilience and building protective habits. Modern research points to several effective strategies:
1. Individualized Trigger Avoidance
Example: People with celiac disease can avoid exposure to gluten by reading ingredient labels and selecting certified gluten-free food. In eczema, swapping out fragranced soaps or detergents reduces skin irritation.
2. Medication Adherence
Missing even one dose of controller medication (like inhaled steroids for asthma, or DMARDs for arthritis) sharply increases flare up risk.
Pro Tip: Set reminders or use pill organizers to ensure consistent dosing; Consult with healthcare providers about any side effects before adjusting medications independently.
3. Protective Lifestyle Choices
- Diet: People prone to urticaria (hives) benefit from low-histamine diets; those with chronic pain syndromes often feel better limiting processed food, red meat, and sugar.
- Exercise: Moderate, regular physical activity like gentle yoga, swimming, or walking can reduce inflammatory markers and lower stress, minimizing autoimmune flare ups.
- Hydration: Drinking enough water keeps mucous membranes moist, easing symptoms of asthma and certain skin conditions.
- Sleep: Chronic sleep deprivation increases systemic inflammation; aim for 7-9 hours of quality rest.
4. Stress Reduction and Mindfulness
Mind-body practices like meditation, progressive muscle relaxation, and mindful breathing lower circulating stress hormones that can spark flare ups. In randomized control trials, patients with Crohn's disease or eczema practicing mindfulness reported reduced flare frequency and overall improved quality of life.
5. Environmental Control
- Use hypoallergenic bedding and wash sheets weekly in hot water for allergies and eczema.
- Install air purifiers to trap pollen, dust, and pet dander (Hospital studies show up to a 65% reduction in asthma flares when using HEPA filters).
- Monitor home humidity levels; 40-50% is typical for preventing both mold growth and excessive drying.
Emerging Therapies and Scientific Innovations

Research into the mechanisms behind flare ups is yielding new prevention tools:
Biologic Medications
Targeted therapies like monoclonal antibodies (e.g., dupilumab for eczema, omalizumab for asthma) interrupt inflammatory signaling molecules upstream, reducing flare severity and frequency.
Real-Life Example: Dupilumab, approved by the FDA in 2017, has reduced severe flare ups in eczema by up to 50%, with manageable side effects. Likewise, new biologics for rheumatoid arthritis are enabling some patients to achieve lasting remission and minimal joint damage.
Digital Health Tools
Smart inhalers, continuous glucose monitors, and wearable skin sensors allow people to collect real-time data, predicting flare ups before they fully develop. Early intervention 7such as increasing controller medication rather than reactive rescue therapy 7leads to better overall outcomes.
The Microbiome Frontier
Gut bacteria influence immune responses, particularly in chronic GI and autoimmune disorders. Emerging probiotics and fecal microbiota transplants are being researched to prevent flare ups by rebalancing microbial communities.
How to Build a Personalized Flare Up Action Plan

While general advice is useful, the most effective approach is highly individualized. Here 2s how to develop your own preventative toolkit:
Step 1: Map Your Baseline
Start with a journal or tracking app to record your usual symptoms, medications, daily routines, and any patterns you notice.
Step 2: Identify Triggers
Work systematically:
- Rotate foods or change environmental exposures one at a time and observe outcomes.
- Use symptom flare logs to report changes to your healthcare provider.
Step 3: Collaborative Planning
Regular check-ins with your doctor or specialist allow you to fine-tune prevention strategies as your body and lifestyle evolve.
Step 4: Create Flare Up Protocols
Have an action plan for common triggers:
- Keep an "emergency kit" (e.g., rescue inhaler, antihistamines, cold packs) readily available.
- Set guidelines for when to escalate medical care (thresholds, alarming symptoms).
Step 5: Educate Your Support Circle
Teach family, friends, colleagues, or caretakers how to assist during a flare up. Knowledgeable support can expedite help and reduce the risk of complications.
Debunking Myths About Flare Ups

Myth 1: Flare Ups Are Always Caused by Something You Did
Not true! Genetics, shifting hormones, and random environmental changes can all play a role. Blaming oneself adds unnecessary stress, often exacerbating symptoms further.
Myth 2: Avoiding Exercise Prevents Flare Ups
In most chronic conditions, light to moderate activity helps protect against inflammation. Only in rare instances 7like during active infections or acute joint inflammation 7is rest preferable to gentle movement.
Myth 3: Natural Remedies Always Work Safely
While some supplements and topical remedies are helpful, some can interact with prescribed medications or irritate sensitive systems. Always consult your healthcare practitioner before trying new therapies.
Success Stories: Real People Managing Flare Ups

- Amelia, age 29 (eczema): Documents her meals, skincare routine, and weather conditions. She credits her improvement to weekly moisturizing, hypoallergenic bedding, and regular exercise.
- Javier, age 41 (asthma): Uses smart inhalers tracking medication use. Maintains plants that clean indoor air but avoids high-pollen florals. Reports 70% fewer attacks after installing home air filtration.
- Priya, age 35 (Crohn 2s): Joined a virtual support group and saw notable benefits in daily stress management strategies, enhancing her medication effects.
Their journeys demonstrate that a tailored prevention toolkit is achievable and effective with informed effort and support.
Key Takeaways and Your Next Steps to Prevention

Research continues to reveal new insights behind flare ups 7from cytokine storm cycles to environmental genomics. Yet, the core of flare up prevention remains steadfast: know your condition, engage proactively with your health care, adopt tailored lifestyle adjustments, and harness innovations as they emerge.
Pay attention to your body 2s signals, be proactive about environmental and stress management, and cultivate a network that supports your health goals. By blending the latest science with practical, everyday actions, you 2ll be well equipped to live fully and confidently 7no matter what challenges your condition may bring.
Rate the Post
User Reviews
Other posts in Grilling & Barbecue
Popular Posts