Alzheimers and the Search for Memory Boosting Therapies
29 min read Clear guide to Alzheimer’s memory-boosting therapies, from approved drugs to lifestyle, devices, and trials, explaining evidence, risks, and realistic expectations for patients and caregivers. (0 Reviews)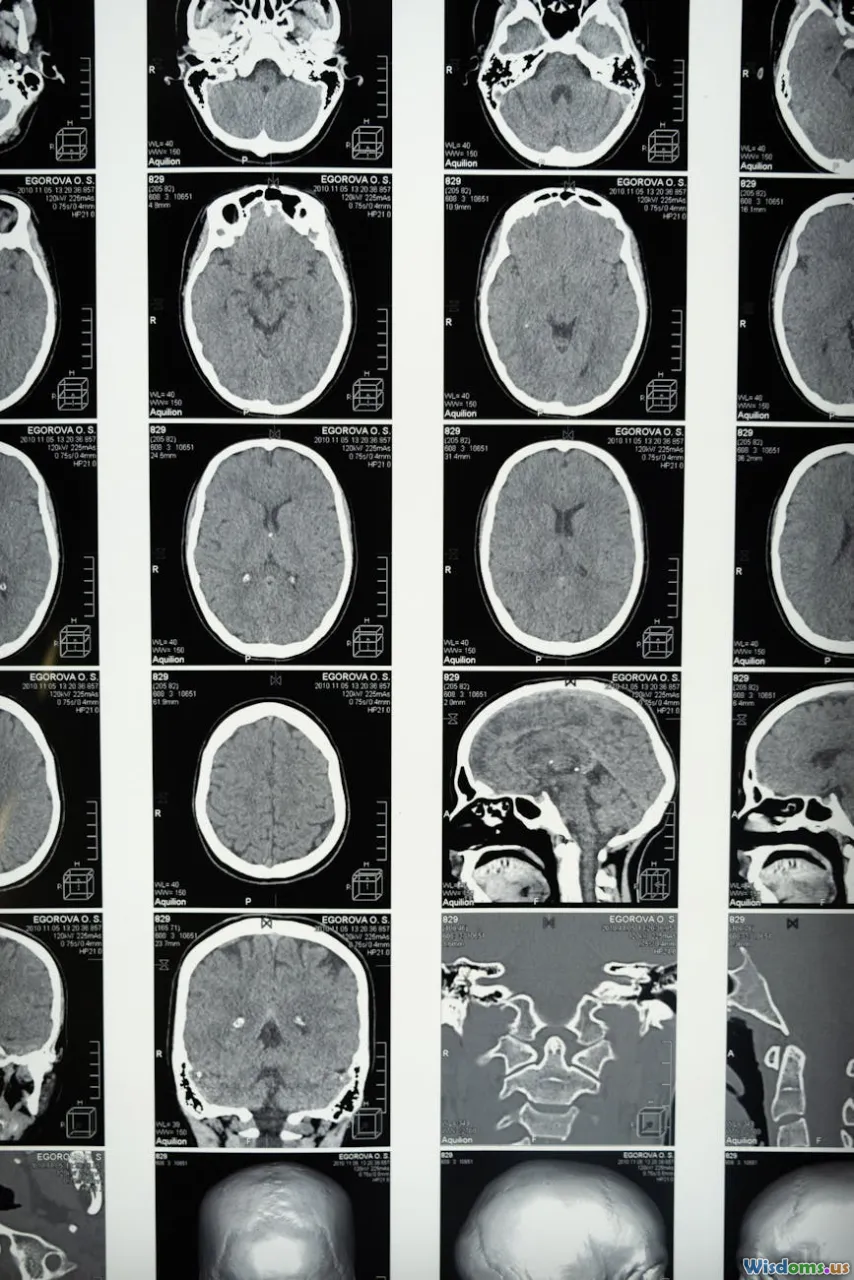
Alzheimer’s and the search for memory-boosting therapies sit at the intersection of hope, hard neuroscience, and everyday practicality. Families want to know what can help today, researchers are revealing why memory unravels in the first place, and new treatments—some headline-making, some quietly effective—are changing what “help” might mean. This article brings those threads together: what memory really is, what current drugs deliver (and what they don’t), the next generation of therapies, and concrete steps that can protect cognition and support day-to-day life.
What Are We Trying to Boost? Understanding Memory in Alzheimer’s

Memory is not a single system. To make sense of “boosting memory,” it helps to map out what Alzheimer’s disease (AD) tends to erode first.
- Episodic memory: Personal events—what you had for breakfast, your grandchild’s recital—live here. It depends heavily on the hippocampus, a structure that shows early AD damage. Trouble recalling recent events is often the first sign noticed by families.
- Working memory: The mental scratchpad that lets you hold a phone number long enough to dial, or follow multi-step directions. This involves frontal networks that can be affected as AD progresses.
- Semantic memory: General knowledge and vocabulary. Relatively preserved in early AD, it can decline later.
- Procedural memory: Skills like riding a bike or typing. Often remains robust longer than other systems.
In practical terms, early AD looks like repeated questions, misplaced items, or difficulty learning new routes. As disease spreads beyond the hippocampus into broader cortical networks (including the default-mode network), organizing tasks, planning, and eventually language can suffer.
Boosting memory may mean different things at different stages:
- In preclinical or prodromal stages, it might mean preserving hippocampal function and slowing pathology.
- In mild-to-moderate stages, it often means enhancing neurochemical signaling and compensating with strategies and environmental supports.
- In later stages, it means minimizing distress and maximizing preserved abilities—leaning on procedural and emotional memory systems.
A key insight: successful “memory support” is rarely one silver bullet. It’s multimodal—combining medical therapy, cardiovascular risk control, environmental design, cognitive training, adequate sleep, and social engagement.
The Current Medicines: What They Do—and Don’t

Two classes of drugs remain the bedrock of symptomatic treatment, while new disease-modifying agents are emerging.
Cholinesterase inhibitors (donepezil, rivastigmine, galantamine)
- What they target: Acetylcholine, a neurotransmitter crucial for attention and memory, is depleted in AD. These drugs inhibit its breakdown, nudging signaling upward.
- What to expect: Modest benefits in attention, memory, and daily activities for some patients, often most noticeable in the first 6–12 months. Effects vary by individual.
- Side effects: Gastrointestinal upset (nausea, diarrhea), vivid dreams, bradycardia in susceptible individuals. Dosing adjustments and transdermal patches can help tolerability.
Memantine
- What it targets: NMDA receptors involved in glutamate signaling. In AD, “noise” in this system may contribute to excitotoxicity.
- What to expect: Modest improvements in cognition and function in moderate-to-severe disease; can reduce agitation in some cases.
- Side effects: Dizziness, headache, constipation; generally well tolerated.
Anti-amyloid monoclonal antibodies (lecanemab/Leqembi, donanemab/Kisunla)
- What they target: Aggregated forms of amyloid-beta that accumulate years before symptoms.
- Evidence so far: In large trials, lecanemab slowed cognitive decline by roughly 27% over 18 months on a standard scale; donanemab showed about 30–35% slowing across key measures in early symptomatic AD. These percentages reflect a slowing of decline, not improvement back to normal.
- Safety and monitoring: Amyloid-related imaging abnormalities (ARIA)—brain edema (ARIA-E) or small hemorrhages (ARIA-H)—occurred in a notable minority of patients, particularly those with an APOE ε4 genotype. Most ARIA is asymptomatic and detected via MRI, but some people develop headaches, confusion, or visual symptoms. These therapies require regular MRIs and infusion-center access.
- Practical realities: Insurance coverage, infusion schedules (typically every 2–4 weeks initially), and eligibility (confirmed amyloid pathology, early disease stage) can be barriers.
What about aducanumab (Aduhelm)?
- Initially granted accelerated approval in 2021, it faced controversy over efficacy. By 2024, commercialization was curtailed, and focus has shifted to agents with clearer benefit-risk profiles.
What “boost” means in practice
- Symptom-focused drugs can improve attention and daily performance, and for some people that feels like a meaningful lift.
- Disease-modifying antibodies can slow the slope of decline, buying time where functions are retained longer.
- None of these are cures. They work best alongside risk-reduction strategies, strong care coordination, and practical memory supports.
Always discuss options with a clinician familiar with dementia care; personal medical conditions, medications, and lifestyle factors influence which therapies make sense.
Beyond Amyloid: The Next Targets in the Pipeline

Alzheimer’s is more than amyloid. A wave of next-generation candidates aims at complementary biology.
Tau-directed therapies
- Rationale: Spread of tau tangles correlates closely with symptom progression.
- Antibodies: Several first-wave anti-tau antibodies failed primary endpoints. Newer approaches target specific tau species or earlier disease stages.
- Antisense oligonucleotides (ASOs): Early studies (e.g., BIIB080/IONIS-MAPTRx) have shown reductions in CSF tau proteins, hinting that gene-level modulation may be feasible. Larger trials will test clinical impact.
Neuroinflammation and microglia
- Microglia, the brain’s immune cells, can be protective or harmful depending on context.
- Targets include TREM2 and complement pathways to rebalance microglial responses.
- The goal: clear toxic aggregates and protect synapses without triggering damaging inflammation.
Synaptic resilience and neurotrophic support
- Strategies to boost brain-derived neurotrophic factor (BDNF) or enhance synaptic plasticity are under exploration.
- Small molecules and peptide mimetics attempt to stabilize connections where memories are encoded.
Metabolic and vascular pathways
- Insulin signaling: Intranasal insulin has shown mixed results; subgroups may benefit. Metabolic modulators (e.g., PPAR agonists) are being studied for people with insulin resistance.
- Cerebrovascular health: Targeting small-vessel disease and blood-brain barrier integrity acknowledges that vascular and neurodegenerative changes often co-occur.
Amyloid production modulators
- BACE inhibitors lowered amyloid but unexpectedly worsened cognition or had unacceptable side effects. Lessons learned: earlier intervention, better selectivity, and combination approaches may be needed—but enthusiasm has cooled.
Protein clearance and proteostasis
- Enhancing autophagy and lysosomal pathways may help dispose of toxic proteins more effectively.
Sensory-driven gamma entrainment
- Nonpharmacologic interventions using 40 Hz light and sound stimulation have shown reductions in amyloid and tau in animal models and early human signals in small studies. Larger, rigorous trials will clarify whether clinical benefits follow.
The likely future: combination therapy. Much like cancer or HIV treatment, tackling AD may require attacking different pathways—amyloid, tau, inflammation, vascular factors—while simultaneously reinforcing synapses and lifestyle systems that make the brain more resilient.
Lifestyle and Risk Reduction: Evidence You Can Use

While no lifestyle step “cures” Alzheimer’s, high-quality trials suggest real, practical gains.
Multidomain programs
- FINGER trial: A 2-year intervention combining exercise, diet, cognitive training, and vascular risk management improved or maintained cognition in older adults at risk compared with general health advice.
- MAPT trial: Mixed overall results, but subgroups with higher dementia risk seemed to benefit from structured multidomain programs.
Blood pressure control
- SPRINT-MIND: Intensive blood pressure control (targeting systolic <120 mm Hg vs <140) reduced the risk of mild cognitive impairment by about 19% and lowered combined risk of MCI/dementia. Implication: what’s good for the heart is good for the brain.
Hearing health
- ACHIEVE trial: In older adults at higher risk of cognitive decline, treating hearing loss with hearing aids and counseling slowed 3-year cognitive decline compared with a control group. If you need hearing aids, using them is a brain-health strategy.
Movement
- Aerobic exercise increases cerebral blood flow, supports white-matter integrity, and is associated with higher BDNF. Even brisk walking 150 minutes/week (e.g., 30 minutes, 5 days) is a strong start.
Diet patterns
- Mediterranean and MIND diets, rich in vegetables, berries, legumes, whole grains, olive oil, nuts, and fish, are repeatedly linked with reduced cognitive decline risk.
- Practical tip: Build your plate with half nonstarchy vegetables, a palm of protein (fish twice weekly if possible), whole grains or legumes, and a thumb of healthy fat (olive oil, nuts).
Sleep and stress
- Regular sleep supports memory consolidation and glymphatic clearance (waste removal). Mindfulness and stress reduction techniques may support attention and mood—both essential for learning and recall.
Smoking and diabetes
- Smoking cessation and tight diabetes control are associated with lower dementia risk. Small improvements in A1C and lipids compound over years.
These steps are not alternative medicine; they are foundational care that often amplifies the benefit of drugs and helps people function better day to day.
Training the Brain: What Cognitive Interventions Can Offer

Cognitive training is not about turning everyone into a Sudoku champion. The most useful programs are targeted and functional.
What tends to work
- Strategy-based training: Techniques like spaced retrieval (practicing recall at increasing intervals), method of loci (memory palaces), and chunking (grouping items) help with names, appointments, and new routines.
- Errorless learning: Reduces encoding of mistakes by guiding correct responses upfront—useful when memory is fragile.
- Goal-oriented rehab: Occupational therapists tailor tasks to daily needs (managing medications, meal prep, travel planning) and build compensatory routines.
Digital tools
- Apps that prompt spaced repetition, smart calendars with location-aware reminders, and voice assistants can serve as “external hippocampi.”
- Evidence: Brain-training games show mixed transfer to real-life tasks; the best outcomes come when training mirrors the tasks you actually do.
Real-world example
- Remembering names at a weekly community group:
- On arrival, take a discreet photo of the seating layout on your phone.
- Pair each new name with a vivid image (Rose → a rose on her shoulder) and say it back once.
- Set a reminder for a 2-minute review that evening using your photo and notes.
- Review again just before the next meeting.
Measure what matters: Track errors missed (e.g., medication skips per month) rather than app scores. If errors drop, the training is working.
Sleep, Memory Consolidation, and Practical Fixes

Memories consolidate during sleep, particularly during slow-wave stages when hippocampal-cortical “dialogue” replays the day’s learning.
Common disruptors
- Sleep apnea fragments sleep and reduces oxygen delivery. Treating apnea with CPAP improves daytime alertness and can stabilize cognition.
- Irregular schedules sabotage circadian rhythms, undermining attention and recall the next day.
Actionable steps
- Stabilize timing: Go to bed and wake within the same 30–45-minute window daily.
- Build a wind-down: 45 minutes of low-light, low-stimulation activity (reading, stretching). Avoid bright screens or use blue-light filters.
- Optimize the room: Cool, dark, quiet. Consider blackout shades and a white-noise machine.
- Caffeine and naps: Avoid caffeine after early afternoon; keep naps short (10–20 minutes) and early.
Emerging ideas
- Acoustic stimulation synchronized to slow-wave sleep can boost deep sleep in lab settings. Consumer versions exist, but clinical impact in AD remains under study.
- Sleep tracking can reveal patterns (frequent awakenings, late bedtimes) worth addressing—but don’t let the tracker become a stressor.
Red flags to discuss with a clinician
- Loud snoring plus daytime sleepiness, acting out dreams, or abrupt changes in sleep patterns warrant evaluation.
Noninvasive Brain Stimulation and Neurotech

Neurostimulation aims to nudge brain networks toward more efficient signaling.
Transcranial direct current stimulation (tDCS)
- Low-current stimulation through scalp electrodes may transiently improve attention and working memory in mild cognitive impairment (MCI) and early AD. Effects are variable and often short-lived; pairing with cognitive training may enhance gains.
Transcranial magnetic stimulation (TMS)
- Repetitive TMS to frontal networks has shown modest benefits for language and executive function in small trials. Protocols vary; benefits, if present, typically require maintenance sessions.
40 Hz sensory stimulation
- Exposing participants to flickering light and sound at gamma frequency (40 Hz) entrained neural activity and reduced pathology in animal models. Early human studies suggest safety and target engagement; definitive cognitive benefits await larger trials.
Deep brain stimulation (DBS)
- Fornix-targeted DBS has been explored; results are mixed, and this remains research-only for AD.
Caveats
- Access and cost are real constraints.
- Stimulation is best considered as an adjunct to foundational care—exercise, sleep, vascular risk control, and cognitive strategies.
Nutrition Supplements and “Nootropics”: Sorting Signal from Noise

The supplement aisle promises a lot. The data are more modest.
Potentially useful in specific contexts
- Omega-3s (DHA/EPA): Observational links exist, but randomized trials in established AD are mixed. More promising when started earlier or in those with low baseline omega-3 status. Aim to get fish in your diet first.
- B vitamins (B12, folate): Treat documented deficiencies. Low B12 can mimic or worsen cognitive issues; correcting a deficiency helps. Routine high-dose supplementation without deficiency hasn’t shown clear benefit in AD.
- Vitamin D: Correct deficiency; broader cognition benefits remain uncertain.
Popular but inconclusive
- Curcumin: Anti-inflammatory and antioxidant effects in theory; bioavailability is an issue. Clinical trials show mixed or small effects.
- Ginkgo biloba: Large trials in older adults did not show prevention of dementia; specific benefits for memory in AD are inconsistent.
- Huperzine A: Acetylcholinesterase inhibition like prescription drugs but less predictable potency and quality control.
- Resveratrol: Mixed results; not a proven therapy for AD.
Metabolic fuels and ketones
- Medium-chain triglycerides (MCTs) and ketone esters can provide an alternative energy source to glucose for neurons. Some small studies suggest cognitive benefits in MCI or in APOE ε4–negative individuals; results are variable, and gastrointestinal side effects are common.
Investigational oral agents
- Amyloid oligomer blockers, tau aggregation inhibitors, insulin-sensitizing compounds, and multimodal metabolic agents are in trials; none should be used off-label outside research settings.
Rules of thumb
- If a supplement “cures” AD in marketing, it’s a red flag.
- Discuss supplements with your clinician to avoid drug interactions (e.g., anticoagulants with ginkgo) and false hopes that delay effective care.
Building a Memory-Supportive Daily Routine

Therapies help most when the day itself is memory-friendly. Small design choices beat willpower.
Create a “cognitive ramp” at home
- One home for essentials: A single tray by the door for keys, wallet, and glasses. Label it.
- Calendar “control center”: A large wall calendar plus a synced digital calendar with shared access for a care partner. Use color-coding: blue for medical, green for social, red for bills.
- Medication mastery: A weekly pill organizer, alarms on phone or smart speaker, and a simple checklist on the fridge. Take meds at the same time as a daily anchor (e.g., breakfast).
Make decisions easier
- Pre-commit menus: Write a 5-day dinner plan on Sunday to avoid daily indecision.
- Pre-pack bags: Keep a small “outing kit” by the door (mask, tissues, notebook, pen, water bottle).
Turn recall into recognition
- Use photos on contact entries so calls and messages carry a face.
- Label drawers and shelves with words plus icons (e.g., a sock symbol) to support semantic and visual memory.
Practice spaced retrieval naturally
- Names: Repeat immediately (“Great to meet you, Rose”), again 1 hour later (text yourself a note), and once before the next event.
- Tasks: Set a cue for 10 minutes, 1 hour, and same time tomorrow. Use the same phrasing: “Lock the back door.”
Reduce cognitive load
- Batch tasks into time blocks (emails 9:00–9:30; bills Thursday 2:00–2:30). Finish one block before starting the next.
- Remove visual clutter from work surfaces; fewer items means less distraction.
Care partner collaboration
- Weekly 15-minute check-in: What worked? What triggered stress? One change for the coming week.
- Share access: Give a trusted person view/edit rights to calendars, medication lists, and important documents.
Biomarkers, Early Detection, and the Ethics of Knowing

We are entering the era of earlier, simpler biomarkers—and bigger decisions about what to do with them.
What’s available
- PET imaging: Amyloid and tau PET can confirm pathology but are expensive and not universally covered.
- CSF tests: Lumbar puncture can measure amyloid and phosphorylated tau with high accuracy.
- Blood tests: Emerging assays (e.g., plasma p-tau217, p-tau181, Aβ42/40 ratio, neurofilament light) increasingly identify AD pathology with good concordance to CSF/PET.
Why it matters
- Anti-amyloid therapies require evidence of amyloid pathology and are intended for early symptomatic stages.
- Biomarkers can clarify diagnosis when symptoms are equivocal.
Ethical considerations
- Psychological impact: Learning about elevated risk or early pathology can cause distress; ensure pre- and post-test counseling.
- Privacy and insurance: Understand how results are stored, who can access them, and potential implications for long-term care insurance.
- Actionability: Know in advance what you’ll do with results—lifestyle changes, clinical trial enrollment, medication decisions—so information empowers rather than paralyzes.
Genetic risk
- APOE ε4 raises risk and influences ARIA risk with monoclonal antibodies. Genetic counseling is advisable before testing.
Clinical Trials: Finding, Qualifying, and Preparing

Trials are where tomorrow’s treatments become today’s options—and often where the most comprehensive care happens.
How to find trials
- Use national registries (e.g., ClinicalTrials.gov) and advocacy organization matchmakers.
- Ask memory clinics; many partner with trial networks and can prescreen quickly.
What to expect
- Screening: Cognitive testing, MRIs, PET or CSF biomarkers, lab work. Expect multiple visits before enrollment.
- Inclusion criteria: Often early-stage AD or MCI due to AD with confirmed amyloid. Some trials focus on prevention in at-risk individuals.
- Commitments: Infusions or injections, MRI monitoring, regular cognitive assessments, and safety labs.
Practical tips
- Logistics: Ask about travel reimbursement, home health options for some visits, and caregiver support stipends.
- Documentation: Keep a single binder (or digital folder) with consent forms, medication lists, adverse-event logs, and contact numbers.
- Questions to ask: “What happens if I have ARIA?” “Can I continue my current medications?” “What is the unblinding policy if the trial ends early?”
Why participate
- Potential access to cutting-edge treatments.
- Intensive monitoring that can catch issues early.
- Contributing to knowledge that benefits others—even if your arm is placebo, your participation sharpens future therapies.
Equity, Cost, and Access: The Real-World Barriers

Therapies that exist only on paper don’t help people. Real-world adoption hinges on cost, infrastructure, and trust.
Costs and logistics
- Infusions require centers, trained staff, and MRI capacity. Rural areas often lack these.
- Copays and prior authorization hurdles can delay care. Financial counseling and patient-assistance programs are essential.
Representation in research
- Historically, minoritized communities have been underrepresented in AD trials, limiting generalizability of results.
- Solutions that work: Community-based recruitment, partnerships with faith and civic organizations, culturally tailored education, and research staff who reflect local communities.
Caregiver economics
- Unpaid caregivers shoulder enormous time and financial burdens. Policies that support respite care, transportation vouchers, and workplace flexibility directly influence adherence to therapies and quality of life.
Technology divide
- Digital tools can help—but only if people have broadband, devices, and training. Libraries, senior centers, and community health workers can bridge these gaps.
What a Credible “Memory Boost” May Look Like in 2030

Projecting forward from current signals, a realistic 2030 model might look like this:
- Personalized risk profiling: A low-cost blood panel (p-tau217, Aβ42/40, neurofilament light), APOE status if desired with counseling, and a vascular/metabolic profile guide your plan.
- Early, time-limited disease modification: If eligible, a course of anti-amyloid therapy (e.g., 12–18 months) initiated at the earliest symptomatic stage—with ARIA risk stratification—followed by surveillance biomarkers. Anti-tau or synaptic-protective add-ons begin to enter the mix.
- Aggressive cardiovascular management: Hypertension, diabetes, sleep apnea, and hearing loss are systematically treated because they significantly influence outcomes.
- Digital-cognitive prescription: A validated, goal-oriented cognitive training program paired with adherence-support apps, wearables that nudge activity and sleep regularity, and secure shared calendars.
- Home design as therapy: Subtle environmental supports—lighting for circadian cues, labels, color-contrast cues for navigation—are standard features rather than afterthoughts.
- Community care teams: Pharmacists, occupational therapists, social workers, and care navigators collaborate so that medical treatments don’t get derailed by transportation, cost, or burnout.
Taken together, this is how “memory boosting” becomes more than a pill: it’s a coordinated system that slows disease processes, strengthens synapses, and makes recall easier through design and habit.
Alzheimer’s is daunting, but it is not static. The field has shifted from whether we can move the needle to how much and how safely—and how to deliver benefits to the many, not the few. For families, the most powerful path blends the best of both worlds: evidence-based medical care and everyday practices that make remembering more likely. Start with what you can control—sleep, blood pressure, hearing, exercise, and a memory-friendly home—and talk with a clinician about eligibility for current medicines or trials. Progress in AD rarely arrives as a miracle. More often, it’s the steady accumulation of small advantages that, together, protect the moments that matter.
Health Neuroscience Cognitive Health Digital Therapeutics Brain Science & Neuroscience Neurodegenerative Diseases Pharmacology Memory Enhancement Aging & Longevity Clinical Trials Alzheimer's disease cognitive decline dementia research amyloid beta tau pathology cholinesterase inhibitors memantine anti-amyloid antibodies biomarkers cognitive training exercise and brain health sleep and memory neuromodulation
Rate the Post
User Reviews
Popular Posts