Diagnosing Memory Loss What Actually Happens in the Brain
8 min read Explore how memory loss is diagnosed and the brain mechanisms behind it with expert insights and practical examples. (0 Reviews)
Diagnosing Memory Loss: What Actually Happens in the Brain
Memory is intrinsically tied to our identity, preserving experiences and knowledge that shape how we navigate the world. So when memory starts to falter, it triggers concern, introspection, and an urgent quest for answers. But what does memory loss really involve within the brain? How do clinicians diagnose it precisely, and what mechanisms are truly at play?
Understanding the process of diagnosing memory loss means peering beyond the superficial symptom to the complex neural circuits and biochemical changes behind it. Let’s embark on a detailed journey that explains how memory works, what goes wrong in the brain to cause forgetfulness, how doctors evaluate these changes, and why early diagnosis is critical.
Understanding Memory and Its Brain Basis
The Architecture of Memory
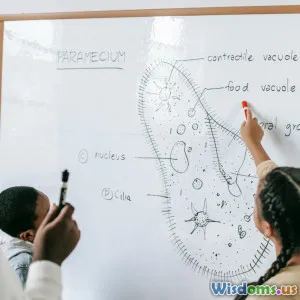
Memory isn’t a single monolith but rather a constellation of types supported by distinct brain regions. Broadly, memory is categorized as:
- Short-term Memory: Holds information temporarily (e.g., remembering a phone number for seconds).
- Working Memory: Actively manipulates information held briefly.
- Long-term Memory: Stores data over extended periods, subdivided into:
- Declarative (explicit) memory: Facts and events.
- Procedural (implicit) memory: Skills and tasks.
The hippocampus, located in the medial temporal lobe, is crucial for the formation of new declarative memories. The prefrontal cortex supports working memory and decision-making. Meanwhile, the cerebellum and basal ganglia underpin procedural memory.
Neural Mechanisms Underlying Memory
At the cellular level, memory formation involves synaptic plasticity—the ability of synapses to strengthen or weaken over time. Long-Term Potentiation (LTP) in the hippocampus is one key process facilitating the consolidation of information from short-term to long-term storage.
Neuromodulators like acetylcholine and glutamate play pivotal roles in enabling effective memory processing. Disruptions in these chemical signaling pathways can impair memory functions.
What Actually Happens in the Brain During Memory Loss?
Common Causes of Memory Loss
Memory loss isn’t a uniform condition but can result from various causes, including:
- Neurodegenerative diseases (Alzheimer’s disease, vascular dementia)
- Traumatic brain injury
- Nutritional deficiencies (e.g., vitamin B12)
- Psychiatric conditions (depression, anxiety)
- Medications and substance abuse
- Sleep disorders
Pathophysiology in Neurodegenerative Memory Loss
In Alzheimer’s disease—the most prevalent cause of pathological memory decline—two hallmark brain pathologies wreak havoc:
- Amyloid-beta plaques: Protein fragments that accumulate extracellularly, disrupting cell communication.
- Neurofibrillary tangles: Twisted fibers of tau protein inside neurons impairing nutrient transport.
These abnormalities first target the hippocampus and adjacent areas responsible for forming new memories, explaining why early symptoms often involve difficulty recalling recent events.
Inflammatory responses and brain atrophy (cell loss) further exacerbate cognitive dysfunction.
Impact on Brain Networks
Memory relies on interconnected networks spread across the brain. Damage interferes with the communication between nodes, particularly between the hippocampus and the neocortex. This breakdown in connectivity diminishes the brain’s capacity to encode, store, and retrieve memories efficiently.
Imaging studies frequently show reduced activity in regions involved in memory and executive control early in disease progression.
How Is Memory Loss Diagnosed?
Clinical Evaluation
The diagnostic journey begins with a nuanced clinical history assessment by healthcare providers:
- Onset, duration, and progression of memory symptoms
- Impact on daily functioning
- Associated symptoms like confusion or mood changes
- Medical and family history
This qualitative context guides subsequent testing.
Cognitive Testing
Standardized tools assess different memory domains and cognitive abilities. Examples include:
- Mini-Mental State Examination (MMSE): Screens global cognitive function.
- Montreal Cognitive Assessment (MoCA): More sensitive for mild cognitive impairment.
- Neuropsychological batteries: Comprehensive tests targeting various memory functions, processing speed, attention, and language.
Quantifying the severity and pattern helps differentiate types of memory loss and underlying causes.
Neuroimaging
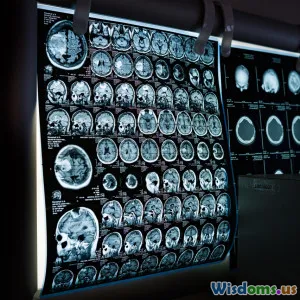
Advances in brain imaging have revolutionized memory diagnostics.
- MRI scans: Reveal structural brain changes like hippocampal atrophy.
- PET scans: Detect amyloid deposits or glucose metabolism deficits indicative of neurodegeneration.
For example, a study published in the Journal of Alzheimer’s Disease (2019) demonstrated that hippocampal volume reduction on MRI correlated strongly with clinical memory decline.
Biomarker Tests
Cerebrospinal fluid (CSF) analysis and blood tests can measure biomarkers such as amyloid-beta and tau proteins, bolstering diagnosis especially in early or ambiguous cases.
Differential Diagnosis
Since many conditions mimic memory loss symptoms, exclusion of reversible causes (e.g., thyroid disorders, depression) through laboratory tests is essential.
Real-World Insights and Advances
Early Detection Importance
Early diagnosis enables timely interventions that may slow progression or improve quality of life. For example, cholinesterase inhibitors can modestly improve cognition in Alzheimer’s if started before extensive brain damage.
Emerging Technologies
Techniques like functional MRI (fMRI), machine learning algorithms analyzing speech/language, and wearable cognitive monitoring devices are pioneering more precise diagnostics.
Patient Stories
Consider Mary, a 68-year-old retired teacher noticed forgetting appointments and struggled recalling recent conversations. Prompt evaluation unveiled mild cognitive impairment, enabling early lifestyle adjustments and therapy that helped maintain her autonomy longer.
Conclusion: The Path from Symptom to Understanding
Diagnosing memory loss is no simple checklist task—it’s an intricate process integrating clinical acumen, cognitive testing, sophisticated imaging, and biology. Knowing what unfolds inside the brain during memory decline provides clarity not only to clinicians but also to patients and families grappling with uncertainty.
These insights spotlight the brain’s extraordinary complexity and resilience while reflecting why timely assessment matters immeasurably. With continued research, enhanced diagnostics promise earlier detection and tailored treatments, shifting the trajectory of memory disorders.
If you or a loved one notice persistent memory changes, consulting a healthcare professional is vital. Because understanding the brain’s story can transform loss into empowerment, resilience, and hope.
Rate the Post
User Reviews
Other posts in Brain Myths and Facts
Popular Posts