Can Neuroplasticity Help Overcome Depression Faster Than Medication
12 min read Exploring how neuroplasticity accelerates depression recovery beyond medication's scope. (0 Reviews)
Can Neuroplasticity Help Overcome Depression Faster Than Medication?
Depression is a complex and often debilitating condition that affects millions of people worldwide. While medication has traditionally been a primary treatment method, recent advances in neuroscience suggest that reshaping the brain through neuroplasticity might offer faster, more sustainable recovery. But is this hope justified? This article delves deeply into the science of neuroplasticity, its potential to accelerate overcoming depression, and how it compares with conventional medication.
Introduction
Imagine your brain as a vast, dynamic network constantly remodeling itself with every experience, thought, or emotion. This capacity—known as neuroplasticity—means the brain isn’t static but is exquisitely adaptable throughout life. For depression, a condition frequently associated with maladaptive neural circuits and negative thought patterns, this adaptability opens an empowering door. Can leveraging neuroplasticity bypass or even outperform the slower pathways of medication?
By exploring evidence-backed neural changes, cutting-edge therapies, and patient stories, this article examines how neuroplasticity-focused interventions might help individuals recover from depression faster and potentially more completely than traditional pharmaceutical treatments.
Understanding Depression: The Brain’s Role
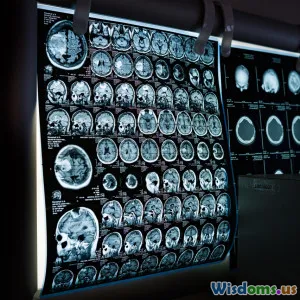
The Neurobiology of Depression
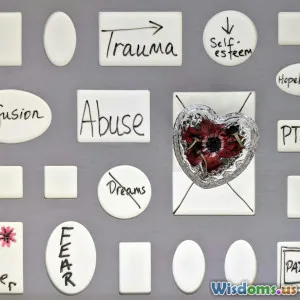
Depression is closely tied to brain chemistry and structure. Common scientific findings show:
- Imbalanced neurotransmitters: Such as serotonin, dopamine, and norepinephrine, which influence mood regulation.
- Altered neural connectivity: Particularly in the prefrontal cortex, hippocampus, and amygdala - regions involved in mood, memory, and stress.
- Reduced neurogenesis: The formation of new neurons, especially in the hippocampus, often declines in depressed individuals.
These factors combine to foster pervasive negative thinking, emotional numbness, and an impaired ability to experience pleasure—hallmarks of depression.
Limitations of Medication
Antidepressants, such as SSRIs and SNRIs, aim to rebalance neurotransmitters. However:
- Delayed onset: Effective symptom relief can take 4-6 weeks or longer.
- Partial or no response: About 30-40% of patients do not achieve remission with medication alone.
- Side effects: Including weight gain, sexual dysfunction, and emotional blunting, which can deter adherence.
These limitations fuel the search for alternative or complementary strategies.
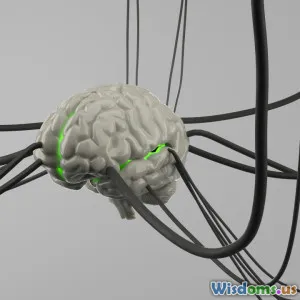
What Is Neuroplasticity and How Does It Work?
Neuroplasticity is the brain’s ability to reorganize neural pathways in response to learning, experience, or injury. There are two main types:
- Structural plasticity: Creating new neurons or strengthening synaptic connections.
- Functional plasticity: Shifting functions from damaged to undamaged brain areas.
Remarkably, neuroplasticity persists across adulthood, which means the depressed brain can potentially rewire itself towards healthier functioning.
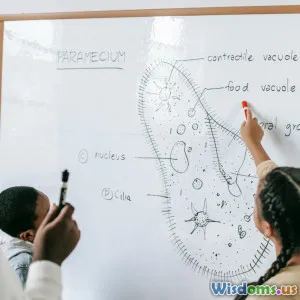
Real-World Example: London Taxi Drivers
Research on London taxi drivers revealed significant grey matter volume increase in the hippocampus—a brain area associated with memory—after extensive spatial-navigation training. This striking proof shows experience can physically alter brain structure.
Similarly, targeted cognitive and behavioral training aimed at depression could remodel maladaptive brain circuits.
Can Neuroplasticity Accelerate Recovery from Depression?
Mechanisms Behind Recovery
Rehabilitation of neural circuits through consistent positive experiences and behaviors can promote:
- Increased neurogenesis: Especially via physical exercise and enriched environments.
- Synaptic strengthening: Through cognitive therapies that retrain thought patterns.
- Enhanced brain connectivity: Improving emotional regulation and resilience.
Evidence from Behavioral Interventions
- Cognitive Behavioral Therapy (CBT):
Multiple imaging studies demonstrate CBT changes activation patterns in the prefrontal cortex and amygdala, correlating with symptom improvement. For example, a 2016 study using fMRI documented reduced hyperactivity in fear-processing centers after 12 weeks of CBT.
- Mindfulness and Meditation:
Regular mindfulness practice has been shown to increase cortical thickness in regions tied to attention and emotion regulation. A 2018 meta-analysis linked mindfulness to elevated hippocampal volume in depressed patients.
- Physical Exercise:
Aerobic activity not only boosts mood biochemically but also promotes growth factors associated with neuroplasticity, such as BDNF (brain-derived neurotrophic factor). Exercise-based interventions have resulted in faster symptom relief and neurogenesis compared to sedentary controls.
Examples of Accelerated Recovery
-
Daniel Siegel, MD, renowned psychiatrist, highlights: "Neuroplasticity offers a conceptual framework for how psychotherapy can literally change the brain, often yielding results in weeks instead of months or years."
-
Clinical trials integrating neuroplasticity principles with treatments like CBT and exercise showed patients achieving remission weeks earlier than those receiving medication alone.
Comparisons: Neuroplasticity-Based Approaches vs Medication
| Aspect | Medication | Neuroplasticity-Based Approaches |
|---|---|---|
| Onset of effects | 4-8 weeks (sometimes longer) | Often within weeks; varies by intervention |
| Mechanism | Alters neurotransmitter levels | Restructures neural circuits |
| Side effects | Common and sometimes serious | Minimal; mostly related to effort and engagement |
| Sustainability | Relapse risk if medication stops | Potentially durable due to lasting brain changes |
| Accessibility | Widely prescribed, covered by insurance | May require commitment to therapy and practice |
While medication primarily modulates chemicals, neuroplasticity leverages behavior and experience-driven brain restructuring, often leading to more sustainable remission and fewer adverse effects.
Limitations and the Need for Integrated Care
Despite promising evidence, it's important to recognize that neuroplasticity-based interventions may not be a stand-in for medication in all cases:
- Severity matters: In acute, severe depression, medications are often life-saving and essential.
- Time, effort, and access: Neuroplasticity interventions like psychotherapy or exercise require consistent time and patient engagement, which might be challenging.
- Individual variability: Genetic and environmental factors influence responsiveness.
Therefore, an integrative approach combining medication for initial stabilization and neuroplasticity-driven therapies for long-term recovery could offer the best outcomes.
Practical Ways to Harness Neuroplasticity for Battling Depression
-
Engage in Regular Physical Exercise: Aim for 30 minutes daily; aerobic activities enhance BDNF, improving mood and brain plasticity.
-
Practice Mindfulness Meditation: Start with short sessions, gradually building to daily routines for emotional regulation.
-
Cognitive Behavioral Therapy (CBT): Professional guidance can restructure negative thought patterns and strengthen adaptive brain networks.
-
Learn New Skills or Hobbies: Challenging the brain with new tasks encourages synaptic growth.
-
Social Connection: Positive social interactions stimulate brain regions impaired by depression.
Empowering individuals with such tools complements medication or, in some cases, offers a meaningful pathway forward.
Conclusion
Neuroplasticity reveals the brain's remarkable ability to heal itself by reorganizing neural pathways. Scientific advances highlight that leveraging this adaptability can accelerate recovery from depression faster than medication alone, especially through therapies encouraging positive behavioral change and brain rewiring.
While medication remains a crucial component for many, particularly in acute phases, integrating neuroplasticity-driven interventions offers a promising frontier. It fosters not only faster but often more durable remission by targeting the root neural circuits of depression.
In essence, understanding and harnessing neuroplasticity places hope firmly back in human hands—not just through pills but through conscious experiences, choices, and persistent healing.
The road to overcoming depression is deeply personal, but nurturing our brains’ inherent plasticity could illuminate the way beyond waiting weeks for medication's effects—toward faster, empowering mental health transformation.
References:
- Hölzel, B. K., Lazar, S. W., Gard, T., et al. (2011). How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspectives on Psychological Science.
- Kumar, P., & Frey, B. (2020). Neuroplasticity and Exercise in Depression Recovery. Frontiers in Psychiatry.
- DeRubeis, R. J., Siegle, G. J., & Hollon, S. D. (2008). Cognitive Therapy vs Medications in the Treatment of Moderate to Severe Depression. The Canadian Journal of Psychiatry.
- Lazar, S. W., Kerr, C. E., Wasserman, R. H., et al. (2005). Meditation experience is associated with increased cortical thickness. Neuroreport.
- Liston, C., Miller, M. M., Goldwater, D. S., et al. (2014). Psychosocial stress reversibly disrupts prefrontal processing and attentional control. Proceedings of the National Academy of Sciences.
Rate the Post
User Reviews
Popular Posts