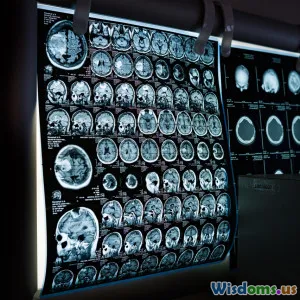
Five Innovative Brain Imaging Techniques Transforming Mental Health Care
15 min read Discover five transformative brain imaging technologies reshaping diagnosis and treatment in mental health care, from fMRI to MEG, with real-world examples and patient impact. (0 Reviews)
Five Innovative Brain Imaging Techniques Transforming Mental Health Care
Introduction: The New Frontier of Mental Health Diagnosis
Imagine a world where we could peer into the living brain and identify the roots of mental distress — from severe depression to schizophrenia — as clearly as seeing a fractured bone on an X-ray. For decades, mental health care advanced through observation, talk therapy, and medication, often hindered by trial and error in diagnosis and treatment selection. Today, brain imaging techniques are rapidly changing the field, replacing guesswork with precision and hope.
These pioneering technologies not only map brain structure, but also visualize its complex functions, connections, and even chemistry. From sophisticated MRI scanners to sensors tracking fleeting electromagnetic signals, brain imaging is unlocking unprecedented insight into what goes wrong in mental illnesses, why some patients respond to certain treatments, and how we might one day prevent psychiatric disorders before they take hold.
In this deep dive, we will explore five cutting-edge brain imaging techniques. You'll learn how they work, real-world examples of their impact, the breakthroughs they've enabled, and what the future holds for brain-based mental health care. Join us at the intersection of science, technology, and human well-being — a frontier with the promise to transform millions of lives.
1. Functional Magnetic Resonance Imaging (fMRI): The Workhorse of Brain Function Mapping
While traditional MRI revolutionized our ability to see static brain structures, functional MRI (fMRI) enables us to watch the brain in action. fMRI measures changes in blood flow and oxygenation, signaling which brain areas are more active during mental tasks, emotions, or rest.
How fMRI Works
- fMRI detects the difference between oxygen-rich and oxygen-poor blood — a proxy for neuronal activity.
- When you think, remember, or feel, active brain regions consume more oxygen. fMRI captures this dynamic in astonishing detail.
Mental Health Breakthroughs
- Diagnosing Depression: A 2012 study at the University of Pittsburgh revealed that individuals with major depressive disorder often show less activity in prefrontal and cingulate regions when processing emotions. This discovery validated biological underpinnings of depression for many clinicians.
- Prediction of Treatment Response: Research teams at UCLA and Emory found that baseline fMRI patterns could predict whether patients with depression would respond better to CBT (Cognitive Behavioral Therapy) or medication. This suggests an imminent era of personalized interventions, reducing the heartbreak of trial-and-error approaches.
- Schizophrenia & Bipolar Disorder: Differences in how brain circuits fire, seen on fMRI scans, are helping distinguish between these often-misdiagnosed conditions, enabling more precise treatments.
Notable Insights
Dr. Helen Mayberg, neuropsychiatrist and pioneer of imaging-based biomarkers, says, "The brain doesn't care about the labels we use for psychiatric disorders. fMRI shows us where in the brain functions diverge, guiding targeted therapy."
Limitations
Despite its precision, fMRI is costly, requires patient stillness (tricky for some), and researchers are still translating findings into everyday clinical tools. However, as technology advances and machine learning algorithms assist in interpreting complex data, clinical adoption grows more likely each year.
2. Positron Emission Tomography (PET): Mapping the Brain’s Chemistry
While MRI and fMRI focus on structure and blood flow, Positron Emission Tomography (PET) shines in revealing the brain's neurotransmitter systems and metabolic processes.
How PET Works
- PET scans require injection of small amounts of radioactive tracers designed to bind to specific neurotransmitters (such as serotonin or dopamine) or molecules involved in energy use.
- As these tracers accumulate in targeted brain regions, scanners detect the emitted positrons, constructing a 3D map showing chemical activity unique to every mental state and illness.
Transforming Diagnosis and Research
- Schizophrenia: Decades of PET research reveal abnormal dopamine pathways in people with schizophrenia, especially in the striatum. This evidence led directly to the development of antipsychotic medications modulating dopamine.
- Depression and Serotonin: PET has measured serotonin receptor density — lower levels linked to depression for some patients, supporting the rationale behind selective serotonin reuptake inhibitors (SSRIs).
- Alzheimer’s Disease: While Alzheimer’s is primarily neurological, early PET studies using tracers for amyloid plaques have been invaluable in identifying individuals at risk, foreshadowing a similar approach for psychiatric illnesses.
Clinical Example
A recent collaboration between Columbia University and NIH used PET tracers to study inflammation in the brains of people with major depression. Elevated microglial activation, revealed by PET, prompted new studies of anti-inflammatory therapies—a striking clinical innovation.
PET Scan Limitations and Advances
On the downside, PET requires exposure to mild radioactivity and specialized centers. Promisingly, research into novel tracers and hybrid PET/MRI scanners promises more detailed, safer imaging, potentially available in standard clinical practice in coming years.
3. Magnetoencephalography (MEG): Fast-Tracking the Brain’s Electromagnetic Symphony
Imagine capturing a movie of your brain’s electrical activities in real time, with millisecond accuracy. Magnetoencephalography (MEG) does exactly that, offering an entirely different perspective from MRI or PET.
How MEG Works
- MEG uses sensitive superconducting sensors (SQUIDs) placed near the scalp to detect tiny magnetic fields generated by synchronized neuron firing.
- Unlike fMRI (which measures slow blood flow changes), MEG records immediate, subtle brain dynamics, often used alongside structural imaging for deeper insight.
Breaking New Ground in Mental Health
- Early Detection of Psychosis: In studies at King’s College London, MEG has allowed researchers to track disruptions in connectivity and synchrony among certain networks in teens at risk for psychosis—sometimes up to a year before symptoms manifest. This heralds the future of true early intervention.
- Autism and Brain ‘Noise’: MEG has pinpointed over-synchronization (or hypersynchronization) in sensory regions as a biomarker of autism, currently driving individualized therapies for sensory processing challenges.
- Anxiety Disorders: Variations in the rhythmic oscillations recorded by MEG have distinguished social anxiety from generalized anxiety disorder far earlier than cognitive testing, informing more specific treatments.
Real-World Applications
Finnish medical centers are actively integrating MEG with psychiatric assessment. According to Dr. Veikko Jousmäki of Aalto University, “What used to be hidden in abstract symptoms is now mapped as concrete dysfunctions in cortical rhythms and networks.”
Challenges
MEG remains expensive and is found mostly in research hospitals, but efforts to miniaturize and commercialize the technology could soon decentralize access worldwide.
4. Diffusion Tensor Imaging (DTI): Revealing the Brain’s Highway System
Mental illness has as much to do with the brain’s wiring — its bundles of nerve fibers — as with its gray matter. Diffusion Tensor Imaging (DTI), a specialized MRI technique, provides detailed visualization of these white matter tracts.
How DTI Works
- DTI measures the diffusion of water molecules in brain tissue. Since water moves more easily along nerve pathways than across them, this technique reveals the direction and integrity of neural highways.
- Computer algorithms reconstruct the shape, density, and connectivity of major white matter bundles with high precision.
Impact on Psychiatric Disorders
- Schizophrenia: For decades, clinicians noticed that many symptoms could be explained by disrupted communication between brain regions. DTI shown widespread abnormalities in white matter tracts linking the prefrontal cortex with other brain areas — a likely contributor to the cognitive deficits, hallucinations, and delusions found in schizophrenia.
- Bipolar Disorder: Researchers in Australia recently identified distinctive microstructural changes in white matter fibers among those with bipolar disorder — differing even from those with depression — which may guide treatment and early identification.
- PTSD and Trauma: DTI is revolutionizing our understanding of the chronic effects of trauma on brain wiring, documenting persistent disruptions between memory and emotional regions (like the hippocampus and amygdala) in those with PTSD.
From Laboratory to Clinic
While DTI’s most dramatic advances are in research, the data increasingly guides clinical practice. For example, psychiatrists sometimes use DTI information to distinguish between ADHD, trauma, and mood disorders in treatment-resistant youth, tailoring care and prognosis with increasing confidence.
5. Near-Infrared Spectroscopy (NIRS): Portable Insights into Brain Function
Most brain imaging happens in large, expensive laboratories. But Near-Infrared Spectroscopy (NIRS) is bringing neuroimaging to the bedside, psychiatrist’s office, and even home.
How NIRS Works
- NIRS uses harmless, near-infrared light shone through the scalp. Hemoglobin absorbs this light differently depending on its oxygenation state, allowing detection of local brain activity patterns, much like a simplified, portable fMRI.
- Recent wearable innovations have even embedded NIRS into headbands and caps worn by patients during daily activities.
Mental Health Applications
- Real-World Depression Monitoring: Japanese researchers developed a NIRS protocol for daily depression tracking, correlating drops in frontal lobe oxygenation with symptom worsening. This enables patients and clinicians to intervene rapidly — far more efficiently than monthly appointments.
- Pediatric and Geriatric Use: NIRS is safe, noninvasive, and tolerant of movement, making it ideal for children, people with dementia, and those unable to undergo MRI scans.
- Cognitive Rehabilitation: Clinics in Germany use NIRS for neurofeedback training in people with anxiety or attention disorders, coaching patients to consciously alter their own brain activation patterns.
Limitations
NIRS cannot image deep brain structures and is less detailed than fMRI or PET. But its low cost and portability are rapidly extending neuroimaging’s reach far beyond the research hospital.
Conclusion: Where Brain Imaging Meets Hope — The Mental Health Revolution Underway
Profound breakthroughs rarely come quickly in mental health. But with the advent of innovative brain imaging techniques like fMRI, PET, MEG, DTI, and NIRS, psychiatry’s "invisible illnesses" are becoming visible.
Today, practitioners use these tools to:
- Move beyond symptom checklists to objective biomarkers.
- Predict which treatment will likely help which patient — before medication or therapy trials begin.
- Detect illnesses early, sometimes years before full symptoms emerge.
- Reduce stigma by affirming the biological reality of psychiatric disorders.
The horizon promises even more. As machine learning mines imaging data for subtle patterns, wearable devices democratize home-based brain monitoring, and global collaborations share discoveries, brain imaging stands poised to transform mental health care as deeply as the microscope changed infectious disease.
Yet, with every new image we capture, the lessons are humbling. Mental health is as complex and unique as the brain itself, and when imaging empowers both science and compassion, truly transformative care becomes possible. The task now is to bridge these technological marvels from lab bench to bedside — ensuring access, equity, and the human touch remain inseparable from clinical progress. As we peer into the brain’s mysteries, we reveal new hope for the millions bravely living with mental illness.
Further Reading:
- "The Upward Spiral: Applying Neuroscience to Reverse the Course of Depression" — Alex Korb, PhD
- "Imaging Brain Circuits in Major Depressive Disorder: Toward Biomarkers that Inform Treatment" — National Institute of Mental Health
- "Real-time fMRI neurofeedback in clinical applications" — Nature Reviews Neuroscience
- "The Role of PET in Psychiatry Today and Tomorrow" — European Journal of Nuclear Medicine
- "Advances in MEG: Toward Clinical Applications in Psychiatry" — Nature Reviews Psychiatry
Rate the Post
User Reviews
Popular Posts