Top Five Myths About PTSD and the Brain Debunked
13 min read Discover the truth behind common PTSD myths, exploring how trauma truly affects the brain and breaking down misconceptions with up-to-date science and real-world insights. (0 Reviews)
Top Five Myths About PTSD and the Brain Debunked
Introduction: Shattering the Illusions Surrounding PTSD
When it comes to post-traumatic stress disorder (PTSD), misconceptions are everywhere—from TV dramas to well-meaning conversations. We are regularly shown haunted veterans or presumed permanently “broken” victims in the media, but science paints a far more nuanced picture. How does the trauma of war, violence, accidents, or even childhood neglect impact the brain? Can the effects be permanently etched into our memories, or is recovery truly possible?
In recent years, neuroscience has illuminated what trauma does to the brain, upending longstanding myths and replacing stigma with understanding. By debunking the most common myths, we can not only support those living with PTSD more effectively but also harness emerging hope for healing. Let’s explore the real story behind PTSD and the brain, and help foster a more informed and compassionate world.
Myth #1: PTSD Is a Sign of Weakness — and Only Affects Certain People
The Truth: PTSD Has Biological Roots and Can Affect Anyone
One of the most persistent myths is that only “weak” or emotionally unstable individuals develop PTSD—often implying that those affected lack resilience or strength. This stereotype is particularly damaging in communities such as the military or emergency responders, where seeking help may be wrongly equated with being unfit for service.
Scientific Evidence
Decades of research prove that PTSD is a biological response to trauma—not a character flaw. The disorder can develop when someone is exposed to life-threatening or deeply disturbing events, regardless of their psychological makeup or resolve. According to the U.S. Department of Veterans Affairs, about 7-8% of people will experience PTSD at some point in their lives. Importantly, people of any age, background, or gender can develop PTSD—even those known for having “iron nerves.”
“Susceptibility” Factors
Certain risk factors do make the development of PTSD more likely, such as:
- Previous trauma or childhood adversity
- Lack of social support
- Severity and proximity of trauma
- Genetic predisposition (gene variants affecting stress hormone regulation)
Yet even with these factors, PTSD is not a foregone conclusion. Many people exposed to horrific events do not develop PTSD, while others might after less overtly traumatic experiences.
Real-World Example
After the 2011 Tornado in Joplin, Missouri, both survivors and emergency workers were found to develop PTSD—but there was no link between “toughness” and symptoms. What made the real difference was having access to strong support networks, emphasizing community rather than individual “strength.”
Myth #2: PTSD Permanently Damages the Brain — There’s No Way to Recover
The Truth: The Brain Is Remarkably Resilient and Neuroplastic
Popular media often portrays PTSD as a life sentence, with trauma creating irrevocable changes in brain structure and function. People speak of permanent “scarring” of the mind, but contemporary neuroscience offers a more hopeful perspective.
What Really Happens in the Brain
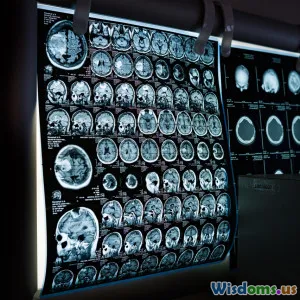
Studies using functional MRI (fMRI) and positron emission tomography (PET) reveal:
- Hippocampus: This region, critical for memory formation, can shrink in people with chronic PTSD. However, recent research (Apfel et al., 2013) found that with successful treatment, the hippocampus size can increase again, suggesting reversibility.
- Amygdala: Heightened activity in this emotion center correlates with hypervigilance and anxiety, but many therapies help to dampen amygdala overactivity step by step.
- Prefrontal cortex: PTSD can reduce activity here, interfering with impulse control and emotional regulation. But brain scans after cognitive behavioral therapy (CBT) often show “normalized” patterns of activity—meaning the brain can heal.
Post-Trauma Resilience
Neuroplasticity—the brain’s ability to rewire itself—is a key factor in healing. With therapies like prolonged exposure therapy, EMDR (Eye Movement Desensitization and Reprocessing), and appropriate medications, many people show significant symptom improvement—with corresponding brain changes.
Quote
“Our brains are not fixed. With the right therapy, many of the structural and functional effects of trauma can be reversed.”
— Dr. Ruth Lanius, Professor of Psychiatry, PTSD Researcher
Inspiring Turnaround
Olympic gymnast Simone Biles, who suffered trauma as a child, openly shared her experience with PTSD and therapy. In interviews, she emphasizes her journey of gradual but tangible recovery: “You learn to cope. It’s not about the trauma defining you, but about coping and healing.”
Myth #3: PTSD Is Always Caused by Just One Major Traumatic Event
The Truth: PTSD Can Stem from Many Forms and Layers of Trauma
A common misconception is that PTSD is only the result of a single, dramatic event—like a battlefield explosion or a car crash. While these are certainly possible triggers, modern psychology and neuroscience acknowledge the complexity and diversity of trauma experiences.
Complex Trauma
Cumulative or “complex trauma”—like ongoing childhood abuse, domestic violence, or chronic exposure to hostile environments—can produce profound symptoms similar to or more severe than “single-incident” trauma. The DSM-5 recognizes both Single-Incident and Complex PTSD (C-PTSD), the latter involving repeated trauma over months or years, often under circumstances where escape is impossible.
Brain Impact
Long-term exposure to toxic stress (e.g., childhood neglect) can alter:
- Default mode network: Implicated in self-perception
- HPA axis: Chronic release of cortisol, the stress hormone, can weaken the immune system and alter neural development if untreated
This is particularly evident in studies with foster children and domestic abuse survivors, where trauma-related symptoms are frequently compounded rather than the result of a single incident.
Examples From the Field
- According to the National Child Traumatic Stress Network, 1 in 4 children exposed to trauma displays PTSD symptomatology, sometimes as a result of ongoing neglect rather than a specific event.
- Military personnel may have “layered trauma,” with older, unaddressed wounds compounding those of recent conflicts.
Key Takeaway
No trauma is too “big” or “small” for PTSD. Repeated microaggressions, neglect, bullying, and invasive procedures can all precipitate trauma responses—making compassion and vigilance essential.
Myth #4: People With PTSD Are Dangerous or Unpredictable
The Truth: PTSD Rarely Correlates With Violence, But Stigma Persists
Perhaps no myth is more damaging than the belief that individuals with PTSD are prone to violent outbursts or unpredictable behavior. This harmful stereotype is inflamed by media reporting and even affects legal proceedings and employment prospects.
What Do the Facts Say?
Multiple large-scale studies—including research from the National Center for PTSD—find no greater risk of violence among those diagnosed with PTSD, compared to the general population. In fact, people with PTSD are far more likely to turn inward, experiencing depression, anxiety, or withdrawal, than to lash out.
Key Data:
- A 2014 meta-analysis (Elbogen et al.) showed that only 9% of veterans with PTSD were involved in physical violence, and most cases were connected to co-occurring substance abuse or lack of treatment—not simply the PTSD diagnosis.
Dangerous Stigma
Stigma doesn’t only affect public perception. It leads to:
- Lower rates of diagnosis (due to fear of being “labelled dangerous”)
- Job discrimination
- Reluctance to seek help, worsening outcomes
Counter-Examples
- Many high-functioning individuals—doctors, firefighters, athletes—manage PTSD Continue to thrive in, and contribute to, their fields without threat to others.
- Peer support projects, such as Wounded Warrior Project, elevate stories that counter the “dangerous” narrative and focus on leadership and collaboration skills developed through trauma recovery.
Myth #5: PTSD Symptoms Never Change or Go Away Over Time
The Truth: Recovery Is Often Gradual — and Possible
A final and persistent myth is that PTSD symptoms are static, fated to remain unchanged for life. This sense of “no escape” can foster hopelessness in those living with the condition.
What the Research Reveals
- Treatment Works: According to the American Psychological Association, 50-70% of individuals with PTSD who receive evidence-based interventions experience significant symptom reduction—many even meeting criteria for full remission.
- Variability Over Time: Longitudinal studies (Kessler et al., 2003) demonstrate that while some symptoms fluctuate, full or partial recovery is the norm—especially when trauma-informed care and social support are present.
- New Frontiers: Advances in psychedelic-assisted therapies, neurofeedback, and virtual reality exposure therapy are providing even more individualized avenues for recovery.
- Brain “Recovery” Is Measurable: PET scans done over 12 months after therapy have shown clear normalization of brain activity in the amygdala, hippocampus, and frontal cortex.
Hope In Practice
Consider Jennifer, a survivor of a catastrophic accident. After years of nightmares and flashbacks, she found relief through trauma-focused cognitive behavioral therapy and yoga. “Over time, I started dreaming again—a different kind of dream. The trauma faded. It’s like my brain recalibrated,” she shared in an NPR interview (2021).
Encouraging Ongoing Support
Recovery is highly individualized. Some people experience slow, subtle improvements; others achieve dramatic change. With compassion, patience, and evidence-based care, most individuals living with PTSD can reclaim their lives and hope.
Conclusion: Moving Toward Trauma-Informed Understanding
The science is clear: PTSD is neither a sign of weakness nor a life sentence, and its effects on the brain—while profound—are often reversible. Debunking common myths allows us to:
- Replace judgment and stigma with empathy
- Guide those in need toward proven, transformative care
- Celebrate recovery stories instead of perpetuating cultural fear
Action Steps for Everyone:
- Learn about available trauma therapies if you or someone you know may be suffering.
- Speak openly to decrease stigma.
- Encourage trauma-informed policies in workplaces and communities.
- Remember, healing from trauma is possible and support makes all the difference.
If you take nothing else from this article, remember: PTSD is not a measure of personal strength, nor is it a life sentence. The brain can heal—and so can you.
Further Resources
Rate the Post
User Reviews
Popular Posts