Comparing Brain Chemistry in Anxiety Versus Depression
10 min read Explore the distinctive brain chemistry differences between anxiety and depression to better understand their symptoms and treatments. (0 Reviews)
Comparing Brain Chemistry in Anxiety Versus Depression
Introduction
Anxiety and depression are often portrayed as overlapping emotional experiences — inseparable companions in the shadows of mental health challenges. Yet, beneath their entwined symptoms lie uniquely nuanced neurobiological landscapes. What precisely differentiates the brain chemistry underlying anxiety from that of depression? Understanding these differences is crucial not only for accurate diagnosis but also for tailoring effective treatments.
In this article, we'll journey deep into the neurochemical underpinnings of anxiety and depression, unraveling the roles of neurotransmitters, neural circuits, and hormonal fluxes. By unpacking evidence-based research and clinical insights, you'll gain a clearer understanding of how brain chemistry intricately influences distinct mental health profiles.
Unpacking Anxiety and Depression: A Brief Overview
Before examining the neurochemical contrasts, it’s essential to define anxiety and depression in clinical terms.
-
Anxiety Disorders are characterized by excessive fear or worry that persists and can lead to physiological symptoms like a racing heart, sweating, or muscle tension. Types include generalized anxiety disorder (GAD), panic disorder, social anxiety, and specific phobias.
-
Depression (Major Depressive Disorder) primarily involves persistent sadness, loss of interest or pleasure in activities, and cognitive and somatic symptoms such as fatigue, changes in appetite, or feelings of worthlessness.
Despite some overlap — many individuals suffer from both — these disorders manifest differently, indicating distinct underlying brain alterations.
Core Neurotransmitters: Serotonin, Norepinephrine, and Dopamine
Neurotransmitters are chemical messengers enabling communication between neurons. They play pivotal roles in regulating mood, arousal, and cognition.
Serotonin (5-HT)
Often dubbed the “feel-good” neurotransmitter, serotonin regulates mood, anxiety, and happiness.
-
In Depression: Reduced serotonergic signaling has long been implicated. The serotonin deficiency hypothesis, while evolving, frames the success of selective serotonin reuptake inhibitors (SSRIs). Studies using PET scans reveal decreased serotonin transporter availability in depressed patients, correlating with severity.
-
In Anxiety: Serotonin plays a modulatory role. For example, altered serotonergic function, particularly in the amygdala—key for processing fear—can increase anxiety levels. Selective activation or blockade of certain 5-HT receptor subtypes leads to anxiolytic or anxiogenic effects.
Norepinephrine (NE)
This neurotransmitter is crucial for arousal, alertness, and the body’s fight-or-flight response.
-
In Depression: Dysregulation of NE pathways is linked to symptoms like lethargy and impaired concentration. Some antidepressants target noradrenergic systems, highlighting this pathway’s importance.
-
In Anxiety: Heightened noradrenergic activity often contributes to hyperarousal and increased heart rate observed in anxiety disorders. The locus coeruleus, a small brainstem nucleus, is a primary source of NE and tends to be overactive during anxiety states.
Dopamine (DA)
Dopamine governs pleasure, reward, and motivation.
-
In Depression: Reduced dopaminergic activity is strongly associated with anhedonia—the inability to feel pleasure—and psychomotor retardation in major depression.
-
In Anxiety: Dopamine’s role is more complex. In some anxiety subtypes (like social anxiety), dysregulation in dopamine balance influences avoidance and fear responses. However, dopamine’s impact is less dominant than serotonin or norepinephrine in typical anxiety presentations.
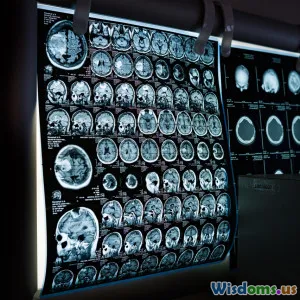
Brain Regions Engaged: Amygdala, Prefrontal Cortex, and Hippocampus
The chemistry differences are reflected in the function of specific brain areas.
Amygdala
Known as the brain’s fear center, the amygdala is hyperactive in anxiety disorders, processing threats and initiating fear responses.
-
Imaging studies show exaggerated amygdala activation during exposure to fearful stimuli in patients with generalized anxiety disorder or post-traumatic stress disorder (PTSD).
-
In depression, the amygdala may also show increased activity, but often coupled with abnormal connectivity in regulatory networks, influencing mood regulation.
Prefrontal Cortex (PFC)
The PFC supervises executive functions and emotional regulation.
-
In Anxiety: Hypoactivation of the ventromedial PFC interlinks with insufficient inhibition over the amygdala, perpetuating anxiety symptoms.
-
In Depression: The dorsolateral PFC is frequently underactive, correlating with impaired decision-making and concentration difficulties.
Hippocampus
Integral to memory and stress regulation, the hippocampus is sensitive to chronic stress.
-
Depression is linked to hippocampal volume reduction, often attributed to elevated cortisol damaging neurons.
-
Anxiety disorders show variable hippocampal findings; for example, heightened volume in certain anxiety states might represent neural compensation.
The Role of the Hypothalamic-Pituitary-Adrenal (HPA) Axis
The HPA axis modulates the body’s stress response by releasing cortisol.
-
In Depression: Many patients exhibit hyperactivity of the HPA axis with elevated cortisol levels, which is linked to hippocampal atrophy and mood disturbances.
-
In Anxiety: Dysregulation of the HPA axis can manifest as an exaggerated cortisol response to stress, particularly in panic disorder and PTSD, sustaining anxiety symptoms.
This hormonal overlap reveals shared mechanisms but diverging patterns of stress response.
Genetic and Environmental Influences on Brain Chemistry
Research underscores that both genetic predisposition and environmental factors shape neurotransmitter systems and brain circuitry.
-
Twin studies estimate heritability of anxiety disorders at about 30-40%, whereas depression can reach up to 40-50%.
-
Early-life stress impacts serotonergic and HPA axis function, predisposing individuals to both conditions but potentially skewing toward depression or anxiety depending on timing and severity.
-
Epigenetic modifications further refine gene expression related to neurotransmitter synthesis and receptor sensitivity.
Implications for Treatment
Pharmacological Interventions
-
Anxiety: Benzodiazepines offer acute relief by potentiating GABA (gamma-aminobutyric acid), the main inhibitory neurotransmitter. SSRIs and SNRIs rebalance serotonin and norepinephrine for long-term management.
-
Depression: Antidepressants mostly target serotonergic and noradrenergic systems. Novel agents such as ketamine target glutamate and show rapid symptom improvement.
Understanding brain chemistry nuances guides personalized medication choices, optimizing effectiveness and minimizing side effects.
Psychotherapy and Neuroplasticity
Cognitive-behavioral therapy (CBT) targets maladaptive neural circuits, promoting neuroplasticity.
Studies demonstrate that psychotherapy can normalize amygdala and PFC activity patterns, illustrating brain chemistry's plastic nature.
Emerging Therapies
-
Transcranial magnetic stimulation (TMS) modulates brain regions like the PFC, beneficial in treatment-resistant depression and some anxiety disorders.
-
Research into gut-brain axis and microbiome suggests future avenues to modify brain chemistry indirectly.
Conclusion
While anxiety and depression often coexist and share some symptoms, their brain chemistry differs in critical ways that illuminate the pathophysiology of each. Distinct neurotransmitter imbalances, varying brain region activations, differential stress hormone responses, and genetic-environmental interplay all contribute to their unique clinical identities.
Comprehending these complexities fosters better diagnostic precision and drives innovative, targeted treatments that address not just symptoms, but the neurochemical roots of these pervasive mental health disorders. By embracing this nuanced understanding, clinicians, researchers, and patients can collaboratively pursue improved mental wellbeing scalability.
References
- Hariri, A. R., & Holmes, A. (2015). Genetics of Emotional Regulation: The Role of Serotonin and Dopamine. Biological Psychiatry, 77(10), 877-887.
- Ressler, K. J., & Mayberg, H. S. (2007). Targeting Abnormal Neural Circuits in Mood and Anxiety Disorders: From the Laboratory to the Clinic. Nature Neuroscience, 10(9), 1116-1124.
- Ball, T. M., Mitchell, C., & Foti, D. (2021). Neurobiological perspectives on anxiety and depression. Journal of Clinical Psychology, 77(6), 1459-1475.
- Savitz, J., & Drevets, W. C. (2020). Neuroreceptor Imaging in Depression and Anxiety Disorders: A Progress Report. Progress in Brain Research, 248, 27-57.
Note: This article is intended for informational purposes and should not replace professional medical advice.
Rate the Post
User Reviews
Popular Posts